- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Can't Step Out Without Your Headphones? They Might Be Damaging Your Brain

Headphones (Credit: Canva)
Can't leave your house without your earphones, airpods or headphones? Well, you aren't alone. There are millions of others who feel the same. However, do not be surprised if I tell you that it may lead to memory loss and dementia. According to the National Library of Medicine, the auditory nerve, which carries sound signals to the brain, when constantly bombarded with loud noises, starts transmitting weaker signals. This forces the brain to work harder to interpret the sound, leading to cognitive overload. Prolonged cognitive strain can eventually pave the way for dementia and memory loss.
Long-term headphone use also affects brain function directly. High decibel levels of noise can damage the insulation of nerve fibres that carry auditory signals to the brain, disrupting the flow of information. Moreover, the electromagnetic waves produced by headphones have been linked to problems like headaches, fatigue, and, in some cases, neurological discomfort.
Beyond The Brain, Headphones Can Make You Deaf
Empirical evidence shows that nearly one billion young people are at risk of hearing loss due to excessive exposure to loud music through headphones. For the uninitiated, sound intensity is measured in decibels. Prolonged exposure to noise above 85 decibels can be harmful to hearing. Music listened to at maximum volume using headphones often falls in the range of 85 to 120 decibels, a level capable of causing significant hearing damage over time.
Studies Show The Ill Effects
According to a recent survey in the UK, a staggering 65% of students admitted to listening to music at maximum volume through their headphones. A similar study revealed that adolescents exposed to high noise levels via headphones in noisy environments experienced a hearing loss prevalence of 22.6%. Those who used earphones for 80 minutes or more per day had a hearing loss prevalence of 22.3%. These figures are alarming, especially given how ingrained headphone use has become in daily life.
The ramifications of early-onset hearing loss go far beyond damaged ears. It can also jeopardize your mental health. Hearing loss in youth can set off a chain reaction, leading to social isolation and depression. Over time, it can also escalate and jeopardise your relationships. Ill-fitting headphones add to the woes, causing pain that extends from the inner ear to the jaws and top of the head. They can also lead to ear infections, which eventually hamper cognitive functions.
Protecting hearing and brain health requires a shift in listening habits. Experts recommend keeping the volume below 60 per cent and limiting usage to 60 minutes per day. Investing in noise-cancelling headphones can also help reduce the need to crank up the volume in noisy environments.
Udit Narayan’s First Wife Alleges She Was Forced to Undergo Hysterectomy, Files Police Complaint
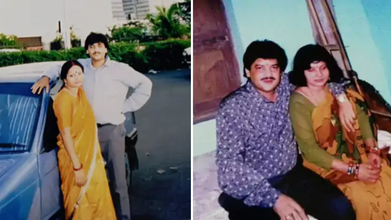
Credits: Facebook
First wife of singer Udit Narayan, Ranjana Narayan Jha made serious allegations against him, claiming that he forced her to get hysterectomy. She filed a police complaint earlier this week at the Women's Police Station in Supaul district, Bihar.
She accused Udit Narayan and his two brothers Sanjay Kumar Jha and Lalit Narayan Jha and his second wife Deepa Narayan of a criminal conspiracy that lead to hysterectomy - the surgical removal of uterus, without her knowledge. As per an NDTV report, "She claimed she became aware of this only years later during medical treatment."
Udit Narayan's First Wife's Allegations
As per the complaint, Udit and Ranjana were married on December 7, 1984, in a traditional Hindu ceremony. Udit then moved to Mumbai in 1985 to pursue his music career. She later learned through media that he had married another woman Deepa. As per the complaint, he continued to mislead her whenever she confronted him.
As per the complaint, in 1996, she was taken to a hospital in Delhi under the pretext of medical treatment, where, she claims that her uterus was removed without her knowledge. She said that she was compelled to file a complaint years after being ignored. "You all know that Udit Narayan ji repeatedly makes promises but does not fulfill them. He has not done anything till now, which is why I have come to the Women's Police Station. I deserve justice," she said.
"Nowadays, I am constantly unwell and need his support. But Udit Narayan is neither saying anything nor doing anything. He came to the village recently and left after making promises once again," she said, as per a Hindustan Times report.
What Is Hysterectomy?
It is the surgical removal of one's uterus and cervix. There are different kinds of hysterectomy available, which depends on the condition of the patients.
Total Hysterectomy
This removes uterus and cervix, but leaves ovaries. This means the person does not enter menopause after the surgery.
Supracervical Hysterectomy
Removing just the upper part of the uterus and leaving the cervix. This could also be when your fallopian tubes and ovaries are removed at the same time. Since, you have a cervix, you will still need Pap smears.
Total Hysterectomy With Bilateral Salpingo-oophorectomy
This is the removal of uterus, cervix, fallopian tubes and ovaries. This will start menopause immediately after the surgery.
Radical Hysterectomy With Bilateral Salpingo-oophorectomy
This is the removal of uterus, cervix, fallopian tubes, ovaries, the upper portion of your vagina, and some surrounding tissue and lymph nodes. This is done to people with cancer. Patients who get this enter menopause right after the surgery.
Lorna Luxe's Husband John Dies After Three Year Long Cancer Battle

Credits: Instagram
Lorna Luxe's Husband, 64, John Andrews passed away after a three-year-long cancer battle. On February 11, the British influencer shared a post on her Instagram. The 43-year-old wrote: "My beautiful, brave John died yesterday. I am heartbroken. We were together to the every end, at home, in our own bed and holding hands which is exactly what he wanted."
Lorna Luxe's Husband John Dies: What Happened To Him?
John, a former banker, was diagnosed with stage three cancer in 2023. He had been receiving treatment over the last three years. John's cancer also entered remission and it returned in 2024 and spread to his brain.
He underwent a surgery in 2025, however, he was back in hospital in December after a complication with his chemotherapy treatments. This led to organ failure.
In January this year, Lorna told her followers that she was "looking for a miracle" and shared that his cancer had "progressed to his other organs" and treatment was "no longer an option".
“I think he's possibly the bravest person. And I suppose at this point we're looking for a bit of a miracle and we're going to take each day as it comes,” she wrote on her post.
In her post that announced John's death, she wrote when she asked him how he was feeling, her husband responded, "Rough, but in love".
Read: Catherine O'Hara Cause Of Death Is Pulmonary Embolism; She Also Had Rectal Cancer
Lorna Luxe's Husband John Dies: Can Cancer Spread To Other Organs?
While John's cancer has not been specified, but the reports reveal that his cancer spread to other organs. According to National Institution of Health (NIH), US, the spreading of cancer to other parts of the body is called metastasis.
This happens when cancer cells break away from where they first formed, and travel through the blood or lymph system. This could lead to formation of new tumors in other parts of the body. Cancer can spread to anywhere in the body, however, it is common for cancer to move into your bones, liver, or lungs.
When these new tumors are found, they are made of the same cells from the original tumor. Which means, if someone has lung cancer and it spread to brain, the cells do not look like brain cancer. This means that the cancer cells in the brain is metastatic lung cancer.
Cancer cells could also be sent to lab to know the origin of the cell. Knowing the type of cancer helps in better treatment plan.
Lorna Luxe's Husband John Dies: Could Chemotherapy Lead To Organ Damage?
As per the University of Rochester Medical Center, in some cases, chemotherapy could cause permanent changes or damage to the heart, lungs, nerves, kidneys, and reproductive organs or other organs.
For instance, some anti-cancer drugs cause bladder irritation, it could result in temporary or permanent damage to kidneys or bladder. In other cases, chemotherapy could also have potential effects on nerves and muscles. Chemotherapy could also damage the chromosomes in the sperm, which could also lead to birth defects. In females, it could damage the ovaries and could result in short-term or long-term fertility issues.
Chemotherapy could also induce menopause before the correct age and could cause symptoms like hot flashes, dry vaginal tissues, sweating, and more.
For some, it could also cause a 'chemo-brain', which is a mental fog that many chemotherapy patients face, that could affect memory or concentration.
Bijou Phillips Hospitalized, Says She Needs Urgent Kidney Transplant: “Time Is Of Essence”

Bijou Phillips Hospitalized, Needs An Urgent Kidney Transplant, Says ‘Time Is Of Essence’(bijouphillips/instagram)
Actress Bijou Phillips, 45, has turned to social media to seek a kidney, issuing an urgent request. In a recent social media post, the ‘Made for Each Other’ actress issued a heartfelt plea for a living kidney donor to help her navigate a the medical crisis.
Phillips framed her request not just as an actress, but through the lens of her family roles. "I’m asking as a friend, a sister, an aunt and most important, a single mother to an incredible and brave daughter," she said.
Why Does Bijou Phillips Need A Kidney Transplant?
In a post dated February 11, she explained that she was born with underdeveloped kidneys and spent 3 months in the NICU (Neonatal Intensive Care Unit). In 2017 she received her first kidney transplant which helped her for eight years. However, she faced many complications including the BK virus that led to cellular and antibody rejection.
BK virus, according to the National Kidney Foundation, is a common inactive virus in the body that can ‘wake up’ after a transplant.
It can cause blurred vision, change in the color of urine, pain or discomfort while urinating, trouble breathing, fever, muscle pain, frequent urination, as well as seizures.
What Causes Underdeveloped Kidneys?
Different conditions are known to cause either underdeveloped kidneys or the absence of one or both kidneys, Bilateral Renal Agenesis/Hypoplasia/Dysplasia. According to the PLOS One 2010 study, these 3 types of underdeveloped kidneys fall under the Congenital Anomalies of the Kidney and Urinary Tract or CAKUT. However there are a few differences.
Bilateral Renal Agenesis
This occurs when both kidneys fail to develop entirely. The study links this to "gene-free" chromosomal breaks and mutations in the Esrrg gene, which normally directs essential early kidney formation.
Renal Hypoplasia
The kidneys are present but significantly small or "underdeveloped." The research suggests this happens when genetic signals for "ductal tissue" are interrupted, preventing the kidneys from reaching their full, functional size.
Renal Dysplasia
This is an "abnormal" formation where kidney tissue is malformed. The study associates this with "laterality" errors, where the body's internal organization fails, causing kidneys to grow with structural defects.
What Are Signs of Underdeveloped Kidneys?
According to the Children’s Hospital of Philadelphia, kidney and urinary tract issues are usually spotted during a pregnancy ultrasound. When a problem is found, doctors watch the amniotic fluid levels closely, since that fluid is mostly made of the baby’s urine. If the issue isn't caught before birth, you might notice these signs in a baby or child:
- Frequent UTIs
- A swollen stomach
- Puffiness
- Stomach troubles
- Slow growth
- Low energy
Bijou Phillips’ Message For Supporters
Currently back on dialysis, Phillips is under the care of Dr. Anjay Rastogi at UCLA. She is actively searching for a living donor and has directed interested individuals to a screening link in her Instagram bio.
"Please help me find a living donor so that I can have more time with my daughter, family, friends," she wrote, expressing deep gratitude for the public's ongoing support.
© 2024 Bennett, Coleman & Company Limited

