- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Health Risks for Ageing Parents: Expert Tells How to Care for Them

Credits: Pexels
As you grow old, your health starts to deteriorate. Everything, whether it is your mental health or your physical health, starts to slow down. However, with age, your mental health gets overshadowed by your physical health.
Signs You Should Note
Neha Sinha, a dementia specialist and CEO and Co-founder of Epoch Elder Care, with the experience of 15 years notes that with age accessing social spaces becomes a hassle. “You are not able to go out because it is not accessible anymore or is not safe. This leads to loneliness. You start to withdraw from all social gatherings, and this leads to a deterioration in your mental health,” she points out.If you note these signs in your ageing parents or grandparents, take note of it. Try to get involved with them. It is also important to ensure that they have a separate social circle apart from the family. This way, they can have friends who they can also relate to.
With age, suggests Sinha, you are more prone to be depressed, and anxious. “Mental health conditions like schizophrenia or bipolar disorders are not something that happens when you grow older. You may have been living with these for the last 40 years, but the management differs, she suggests.
As you grow old, your symptoms start to overlap with other mental health conditions. For the proper treatment professionals use differential diagnosis, suggests Sinha. “The lines become blurred and to differentiate the symptoms from one mental health condition to another becomes difficult,” she says.
Preventive Measures
While there are ways like performing brain quizzes and optical illusions to keep your brain functioning, Sinha says that not many studies have been done on it. Thus, it cannot be guaranteed that it will help. However, it surely helps keep your brain active.There are also food habits like eating leafy vegetables, nuts, fish, virgin coconut and beans that help with brain functions.
Sinha suggests that keeping a social circle and continuing your hobbies can help your mind stay healthy. “Men especially face this issue, after they retire, they feel like they are at the loss of authority, and they start to lose control. It is thus important to keep doing things and learning a new skill to keep your brain active. While for women, since they continue taking care of the house, their brain stays active,” she says.
Cognitive stimulation is the key, especially to managing dementia, she notes.
“Just with weight training, you push your body and after a while, it becomes your muscle memory. Same with the brain. However, one should not get into solving too many puzzles, or trivia after being diagnosed with dementia. Because that would mean you are making your already injured brain exercise which might lead to agitation,” she recommends.
How to support?
It is important to know the ways you can support your ageing parents after they have been diagnosed.“The most important part is for the caregiver to understand what is happening and come to terms with the conditions. Because the elderly with cognitive conditions are not able to understand, they cannot be told or instructed to do anything. Thus, the responsibility is solely on the caregiver,” points out Sinha.
So, what can be done?
Awareness
Sinha suggests that the caregiver must understand that most cognitive conditions in ageing parents is progressive. “Even if you give your 200%, the condition will progress, you must not blame yourself for it. But you can delay the progression by creating a healthy environment.”Reach out to therapists and counsellors to know the ways to create such a healthy environment.
Be Patient
With progressive neurological conditions, the capability to communicate also deteriorates. “If you have a million words in your vocabulary, your parents might have a handful. So, it is important to pay attention to their needs,” she says.She suggests adopting the same approach that you do with kids and with your pets. This is when you focus on gestures, body language and mood over language. Due to cognitive disorders, parents experience a loss of language and the only way to communicate and to understand what they are communicating is through these means.
Be Empathetic
The earliest sign of dementia is short-term memory loss. “This means that your parents may not remember what they had or breakfast or if they had breakfast at all. But they will remember their childhood stories. You may be confused if there is at all a memory loss since they remember old stories, and you might think they are doing this on purpose. But this is not the case,” she says.Create a healthy environment by agreeing with them and listening to their stories. The responsibility of creating a safe environment is totally with you.
There might be times when your parents may do socially unacceptable or non-compliance behaviour. But it is important to understand the triggers and ensure that the triggers do not occur anymore.
Help Them Stay Fit
It is important that they physically stay well, and do not get any infections or don’t suffer a fall. For that, you can use the help of technology like motion sensors. GPS tracker is another way you can keep a check on them. “There is a tendency of wandering off and being unable to find your way back. In these cases, a GPS tracker can help,” she says.The 4 Parkinson's Signs That Appear Years Before Diagnosis

Credit: Canva
Parkinson's disease is a progressive, neurodegenerative movement disorder caused by the loss of dopamine-producing brain cells, primarily affecting people over 60. Apart from motor loss, the disease also causes cognitive decline, depression, anxiety and swallowing problems.
The first symptom may be a barely noticeable tremor in just one hand or sometimes a foot or the jaw. Over time, swinging your arms may become difficult and your speech may become soft or slurred. The disorder also causes stiffness, slowing of movement and trouble with balance that raises the risk of falls.
However, before clear symptoms begin to appear, Neurologist Rachel Dolhun says certain signs may help identify the onset of the disease decades before it is diagnosed.
“It’s important to stress that not everyone who has these symptoms goes on to develop Parkinson’s,” said neurologist Rachel Dolhun. “But we know that in some people, these can be some of the earliest signs," she told The Washington Post.
Here is what you should look out for:
1. Loss Of Smell
Loss of smell, or hyposmia, is a common and early non-motor symptom of Parkinson's disease, affecting up to 90 percent of patients. This symptom can significantly impact quality of life by reducing the enjoyment of food and diminishing appetite.
While strongly linked to Parkinson's, smell loss can also stem from other causes, including sinus problems, COVID-19, or aging.
2. Acting Out Dreams
Acting out dreams, known as REM Sleep Behavior Disorder (RBD), involves physically enacting vivid, often unpleasant dreams through shouting, punching, or kicking during sleep.
This typically happens because the brainstem fails to temporarily paralyze muscles during REM sleep. It is a strong early warning sign of Parkinson's disease, often appearing years or decades before motor symptoms. About 50 percent of people with Parkinson's experience RBD.
READ MORE: Parkinson’s Patients May Soon Walk Better With This New Personalized Brain Therapy
3. Constipation
Constipation is a very common and significant non-motor symptom of Parkinson's disease that is caused by nerve changes slowing gut muscles and potentially exacerbated by low activity and dehydration.
Constipation can also be caused by Parkinson's medications such as anticholinergics, amantadine and other common drugs such as opioids, iron/calcium antacids.
4. Dizziness As You Stand
The autonomic nervous system fails to properly constrict blood vessels or increase heart rate upon standing, often due to a lack of norepinephrine. This causes the autonomic nervous system to fail in regulating blood pressure. Over time, this leads to Neurogenic Orthostatic Hypotension.
Beyond dizziness, symptoms include blurred vision, weakness, fatigue, cognitive "fog," and "coat hanger pain" (pain in the neck/shoulders). Often times, patients experience dizziness in the morning or immediately after meals.
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking questions and reviewing your medical history. Various imaging and diagnostic tests used to detect disease includes CT scan, PET scan, MRI scan and genetic testing.
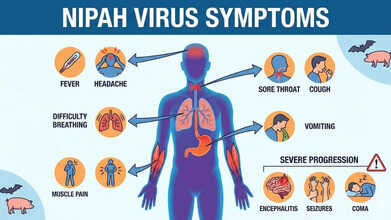
Nipah Virus Symptoms Explained As Doctors Warn Up To 75% Fatality Risk
Credits: AI Generated
Health authorities have urged the public to stay alert to Nipah virus symptoms after doctors warned that up to 75 per cent of infected patients may not survive. The UK Health Security Agency (UKHSA) has classified Nipah as a “high priority pathogen” because of its severe fatality rate and the absence of any proven treatment.
In India, the federal health ministry has confirmed two cases in the eastern state of West Bengal. This has triggered large-scale containment measures, with local officials placing nearly 200 people who had contact with the infected individuals under quarantine.
Also Read: Vitamin D Supplements Under Scrutiny As It Fails Safety Test
In response, several Asian nations have stepped up airport checks and health surveillance for travellers arriving from India. Professor Paul Hunter, an infectious disease specialist at the University of East Anglia, said identifying Nipah cases at borders is challenging, as symptoms can take a long time to appear.
What Is Nipah Virus?
According to UKHSA, Nipah virus is a zoonotic infection, meaning it can pass from animals to humans. It can also spread through contaminated food or via direct human-to-human contact. The virus was first discovered in 1999 during an outbreak affecting pig farmers in Malaysia and Singapore.
Fruit bats, especially those belonging to the Pteropus species, are the virus’s natural carriers. Research shows that Nipah can also infect other animals, such as pigs, dogs, cats, goats, horses and sheep.
Nipah Virus Symptoms
UKHSA lists the following as common symptoms of Nipah virus infection:- Sudden onset of fever or general flu-like illness
- Development of pneumonia and other breathing-related problems
- Swelling or inflammation of the brain (encephalitis) or meningitis
Symptoms usually appear between four and 21 days after exposure, although longer incubation periods have occasionally been reported. More severe complications, including encephalitis or meningitis, can develop between three and 21 days after the initial illness begins.
Also Read: Nipah Virus Outbreak In India: All That You Need To Know About This Infection
Nipah Virus Symptoms Explained As Doctors Warn 75% Fatality Rate
UKHSA has cautioned that between 40 and 75 per cent of people infected with Nipah virus may die. Those who survive can experience long-term neurological effects, such as ongoing seizures or changes in behaviour and personality. In rare instances, the virus has been known to reactivate months or even years after the first infection.
Nipah Virus: Can You Prevent It From Spreading?
For people travelling to regions where Nipah is known to occur, prevention largely involves reducing exposure risks:
- avoid contact with bats, their habitats, and sick animals
- do not drink raw or partially fermented date palm sap; if consuming date palm juice, make sure it has been boiled
- wash all fruits well with clean water and peel them before eating; avoid fruits found on the ground or those that appear partly eaten by animals
- use protective clothing and gloves when handling sick animals or during slaughter and culling
- maintain good hand hygiene, especially after caring for or visiting ill individuals
- avoid close, unprotected contact with anyone infected with Nipah virus, including exposure to their blood or bodily fluids
Nipah Virus Symptoms Can Be Transmitted Easily?
Many Nipah infections have been linked to eating fruit or fruit-based products contaminated by the saliva, urine or droppings of infected fruit bats. Human-to-human transmission can also occur through close contact with an infected person or their bodily fluids, according to Mirror.
Such transmission has been documented in India and Bangladesh, with cases often involving family members or caregivers tending to infected patients. At present, there is no specific, proven treatment for Nipah virus infection, and no licensed vaccine is available to prevent it.
So far, no Nipah virus cases have been reported in the United States or the United Kingdom.
People Who Began Smoking Before 20 Face Higher Stroke Risk, Study Shows

Credits: Canva
Smoking has long been recognized as one of the most preventable causes of disease and early death worldwide. It plays a major role in heart attacks, strokes and several chronic illnesses. While public health messaging often focuses on how much a person smokes, new research suggests that when someone starts smoking may be just as important for long-term health.
A large nationwide study published in Scientific Reports analyzed health data from over nine million adults in South Korea. The findings were striking. People who began smoking before the age of 20 faced a significantly higher risk of stroke, heart attack and early death compared to those who started later, even if their total lifetime smoking exposure was similar.
Smoking Before 20: Why the age matters
Traditionally, doctors and researchers estimate smoking-related harm using pack-years, which combines the number of cigarettes smoked per day with the number of years a person has smoked. While this remains useful, the new study highlights an important gap. Two people with the same pack-years may not have the same health risks if one started smoking much earlier in life.
The researchers found that early starters had a much higher risk of stroke and heart attack than those who took up smoking after the age of 20. This suggests that the body may be especially vulnerable to tobacco damage during adolescence and early adulthood, making age of initiation an independent risk factor.
Smoking and stroke: what we already know
The link between smoking and stroke is well established. Long-term studies, including the famous Framingham Heart Study, have consistently shown that smokers are far more likely to experience a stroke than non-smokers. The risk increases with the number of cigarettes smoked and affects people across age groups.
Smoking damages blood vessels, speeds up plaque build-up in arteries, raises blood pressure and makes blood more likely to clot. All of these changes increase the chances of both ischaemic and haemorrhagic strokes. Younger adults who smoke are not protected simply because of their age, and in many cases, their relative risk is even higher.
Key findings from the Korean cohort
The study followed participants for nearly nine years using data from a mandatory national health screening programme. Researchers looked at stroke, heart attack, combined cardiovascular events and overall death rates.
Those who started smoking before 20 had about a 78 percent higher risk of stroke compared to non-smokers, especially when they also had high smoking exposure. Early starters also showed a much greater risk of heart attacks and combined cardiovascular events. Importantly, they had a higher risk of death from all causes, not just heart-related conditions. These patterns were consistent across men and women and across different metabolic health profiles.
Why early smoking causes greater harm
There are several reasons why smoking at a younger age may be more damaging. During adolescence, the heart, blood vessels and brain are still developing, which may make them more sensitive to toxins in tobacco smoke. Starting early is also linked to stronger nicotine dependence, making quitting harder and often leading to longer periods of smoking.
Early exposure may also trigger lasting inflammatory and metabolic changes in the body. These changes can increase stroke risk later in life, even when total cigarette exposure appears similar on paper.
What this means for public health
The findings send a clear message. Preventing smoking during adolescence could significantly reduce the future burden of stroke and heart disease. School-based education, strong warning messages and policies that limit youth access to tobacco remain critical.
Delaying smoking initiation, even by a few years, may have lifelong benefits. With cardiovascular diseases already among the leading causes of death globally, protecting young people from tobacco use is not just about avoiding addiction. It is about safeguarding their long-term health.
© 2024 Bennett, Coleman & Company Limited

