- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Worried About MPOX? Find Out How Quickly Symptoms Develop And What To Do Next
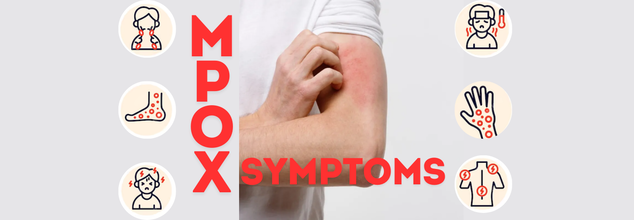
MPOX formerly known as Monkeypox has gained significant attention globally due to its increasing cases and widespread concern. If you're worried about your risk or exposure, understanding how soon symptoms might develop is crucial. Let’s delve into what happens after exposure to MPOX, how the virus manifests, and the necessary steps to protect yourself and others.
As of the latest reports, MPOX cases have been recorded worldwide, with regions like Pak-occupied Kashmir also reporting cases. India remains on high alert as the virus spreads. According to a recent update, there have been significant efforts to monitor and contain the virus, but awareness about its transmission and symptoms remains critical.
What Is MPOX?
MPOX, commonly known as monkeypox, is a rare viral disease that belongs to the orthopoxvirus genus, the same family as the more well-known smallpox virus. Though generally less severe, MPOX can still lead to serious health complications, especially in immunocompromised individuals, children, and pregnant women. The virus is transmitted from animals to humans and can spread from person to person through direct contact with infectious sores, scabs, body fluids, respiratory droplets, or contaminated materials.How Soon After Exposure to MPOX Will Symptoms Appear?
Understanding the timeline from exposure to symptom onset is essential in recognizing and managing the disease effectively. Once you’ve been exposed to MPOX, the virus doesn’t cause symptoms immediately. It has an incubation period—the time between exposure to the virus and the appearance of symptoms—ranging from 5 to 21 days, with most cases presenting symptoms between 3 to 17 days after exposure.During the incubation period, the virus multiplies in the body, but the person remains symptom-free. It’s only after this period that the first signs of MPOX begin to emerge.
Recognizing MPOX Symptoms
The onset of MPOX typically begins with nonspecific symptoms that resemble other viral illnesses, making early detection challenging without testing. The initial symptoms often include:- One of the first signs of MPOX is a sudden rise in body temperature. This fever can range from mild to severe.
- Following the fever, you may experience intense headaches and muscle pains, contributing to overall discomfort.
- The illness may cause profound fatigue, making even simple tasks feel exhausting.
- One of the key distinguishing features of MPOX compared to other poxviruses is lymphadenopathy, or swollen lymph nodes, which often occurs in the neck, armpits, or groin area.
Within a few days of the fever’s onset, the more distinctive rash begins to develop. This rash goes through several stages:
- Macules: Flat, discolored spots appear on the skin.
- Papules: The spots elevate, forming small, raised bumps.
- Vesicles: These bumps fill with clear fluid.
- Pustules: The fluid becomes cloudy and pus-filled.
- Scabs: Finally, the pustules scab over and eventually fall off.
What Should You Do If You Think You’ve Been Exposed to MPOX?
If you believe you’ve been exposed to MPOX, it’s important to monitor your health closely for the next three weeks. Here’s what you should do:1. Self-Isolate
If you develop symptoms, particularly a rash, fever, or swollen lymph nodes, immediately self-isolate to prevent potential spread.
2. Seek Medical Advice
Contact your healthcare provider for advice on testing and next steps. They may recommend getting tested for MPOX, especially if you’ve been in close contact with someone diagnosed with the virus.
3. Avoid Close Contact
While awaiting results or if you have confirmed MPOX, avoid close contact with others, especially those at high risk, such as immunocompromised individuals, children, and pregnant women.
Safety Tips to Protect Yourself and Others
To reduce your risk of contracting or spreading MPOX, practice the following safety measures:- Regularly wash your hands with soap and water or use an alcohol-based hand sanitizer.
- Refrain from close contact with people showing symptoms or those who have been diagnosed with MPOX.
- If caring for someone with MPOX, use personal protective equipment (PPE) such as masks and gloves to minimize your risk.
- Regularly disinfect surfaces and items that may have come into contact with the virus.
Most Medical Videos Even By Doctors Online Are Factually Incorrect, Finds Study

Representational Image by iStock
Most health videos on YouTube, even those made by doctors are also not reliable medical information, found a new study, published in JAMA Network Open. The researchers reviewed 309 popular YouTube videos on cancer and diabetes and found that fewer than 1 in 5 were supported by high quality scientific evidence. About two-thirds of the view had low, very low or no evidence at all to back up their health claims.
What was more concerning is that weaker evidence often attracted more viewer than those backed with strong science. The study looked at videos which had at least 10,000 views. The lead author of the study Dr EunKyo Kang of South Korea's National Cancer Center, said, "This reveals a substantial credibility-evidence gap in medical content videos, where physician authority frequently legitimizes claims lacking robust empirical support."
"Our findings underscore the necessity for evidence-based content-creation guidelines, enhanced science communication training for health care professionals, and algorithmic reforms prioritizing scientific rigor alongside engagement metrics," Kang added in a news release.
How Was The Study Conducted?
The researchers reviewed videos from June 20 and 21, 2025, focusing on cancer and diabetes content. 75 per cent of them were made by physicians. The videos had a median count of 164,000 views and a median length of 19 minutes.
Researchers also developed a scoring system, called E-GRADE to rate the strength of science backed evidence in each video's claim.
This is how the grading system worked:
- GRADE A: high quality evidence
- GRADE B: standard quality evidence
- GRADE C: low quality evidence
- GRADE D: very low or no evidence
What Were The Results Of The Medical Videos?
- GRADE A: 19.7%
- GRABE B: 14.6%
- GRADE C: 3.2%
- GRADE D: 62.5%
The study also found that videos with the weakest evidence were 35% more likely to get higher views than videos with strong scientific evidence.
Richard Saver, a professor of law at the University of North Carolina at Chapel Hill noted that this issue is not just limited to YouTube. "Physician-spread misinformation is a long-standing problem, dating back well before the internet era," he wrote in an accompanying editorial.
Saver said some doctors continue to lean on personal experience rather than solid data, despite evidence-based medicine being regarded as the gold standard. He noted that EBM can feel like it downplays individual clinical judgment. Still, Saver stressed that more research is needed, adding that the study underscores the importance of examining the evidence behind health professionals’ claims on social media.
How Health And Me Has Helped With Medical Facts
Health and Me has always stayed a step ahead from medical misinformation and ensured that its readers too consume correct information. Health and Me's Fact Check series have consistently ran checks on bizarre medical claims, whether it is about a magical potion for weight loss, fake health news, or un-scientific remedies.
Fact Check By Health And Me:
- Fact Check: Does Circumcision Really Cause Autism As Claimed By RFK Jr.?
- Fact Check: Semen Production Means You Have Healthy Sperms, Here's What The Doctor Says
- Fact Check: Is The COVID-19 'Lab Leak' Theory Correct?
- Fact Check: Are Fewer Childhood Vaccines Really “A Better Thing” Under the New CDC Guidelines?
- Fact Check: Is Weight Lifting Safe for Teens? An Expert Explains the Risks and Safer Alternatives
- Fact Check: Do Heart Attacks Peak in the Early Morning? Here’s What a Doctor Says
- Fact Check: Does Ja Morant Have Lung Cancer?
- Fact Check: Can Cold Morning Showers Trigger Brain Stroke?
- Fact Check: Is The Pink Salt Trick Recipe Effective For Weight Loss?
Menopause Clinics Explained: Latest Launch By Maharashtra And Kerala Government

Credits: Canva
The World Health Organization (WHO) noted that menopause often goes unnoticed as a clinical priority, observing these unmet needs, the state governments in Maharashtra and Kerala will soon launch government-run menopause clinics. These clinics will have specialized support systems designed to offer holistic healthcare services for menopausal women within the public system.
These clinics will also have medical consultations, mental health counselling, targeted screening services and lifestyle guidance.
What Are Menopause Clinics?
Menopause clinics are specialized healthcare units, usually housed in government hospitals, urban health centres or district hospitals, that focus on both the medical and emotional needs of women transitioning through menopause. Rather than brushing menopause aside as a “natural” phase that needs little attention, these clinics offer organized, evidence-based care that goes well beyond routine outpatient visits.
At the heart of a menopause clinic is a comprehensive, integrated approach that includes:
- Clinical assessment of menopausal symptoms
- Screening for hormonal and physical health issues, such as bone health and heart disease risk
- Mental health support and psychosocial counselling
- Personalized advice on lifestyle, nutrition and mid-life wellness
- Ongoing patient education and structured follow-up
By bringing these services together under one roof, menopause clinics help women cope with day-to-day symptoms while also addressing long-term risks like osteoporosis, metabolic changes and a higher likelihood of cardiovascular disease.
What Is Menopause?
This is the natural, permanent end of menstruation defined as 12 consecutive months without a period. This typically occurs between ages 45 to 55.
Foods That May Help During Menopause
- Soy: A top source of phytoestrogens, particularly isoflavones, which bind to estrogen receptors in your body. Studies suggest soy may help alleviate hot flashes, improve cholesterol levels, and even reduce the risk of heart disease during menopause.
- Flaxseed: Packed with lignans, a type of phytoestrogen with mild estrogenic effects, flaxseed may also offer some relief.
Including these foods in your diet could help ease symptoms and reduce your risk of certain menopause-related conditions.
Why a Balanced Diet Matters
A nutrient-packed, balanced diet is the foundation of good health at any age. Prioritize:
- Vegetables and fruits: Rich in vitamins and antioxidants.
- Whole grains: Great for maintaining steady blood sugar levels.
- Lean proteins: Support muscle health and repair.
- Low-fat dairy: Provides calcium for bone strength.
- Avoid ultra-processed junk foods, excessive sugar, and unhealthy fats, which contribute little beyond empty calories.
Maharashtra Menopause Clinic
Earlier this January, the Maharashtra government rolled out the country’s first state-run menopause clinics across government hospitals and urban health facilities. The initiative was launched on Makar Sankranti, January 14, under the guidance of Minister of State for Health Meghna Bordikar.
As per official statements, these clinics are designed to offer end-to-end care in one place. Services include expert medical consultations to evaluate and manage menopausal symptoms, mental health support to address emotional and psychological concerns, and screenings for bone health, cardiovascular risk and hormonal balance. Medicines and follow-up advice are also provided during the same visit, cutting down the need for multiple referrals and repeat hospital trips.
A senior health official pointed out that while menopause is a natural life stage and not a disease, many women need consistent physical and emotional support during this transition. The strong response from women across Maharashtra highlights a long-standing gap in healthcare, where menopause-related concerns often went unaddressed due to the absence of dedicated services. With this move, Maharashtra has also set an example for other states looking to introduce gender-specific care within public health systems.
Read: Can Your Diet Affect Menopause?
Kerala follows with dedicated clinics
Taking a cue from Maharashtra, the Kerala government has announced plans to set up specialized menopause clinics in district hospitals. An initial allocation of Rs 3 crore has been earmarked for the project in the 2026 state budget, presented by Finance Minister K N Balagopal.
The proposed clinics in Kerala will follow a similar model, offering medical consultations for menopausal symptoms, mental health counselling, and screenings for heart, bone and hormonal health. Women will also receive medicines along with lifestyle and dietary advice at a single facility.
The initiative acknowledges the wide-ranging impact of menopause, including hormonal changes, sleep disturbances, bone health issues and increased stress, and aims to create a one-stop support system within district hospitals. By bringing menopause care into mainstream public healthcare, Kerala hopes to improve access, reduce stigma and ensure that women receive timely, structured support during this phase of life.
Bruce Willis’ Wife Emma Says He Is Unaware of His Dementia Diagnosis
Credits: Wikimedia Commons
Bruce Willis was diagnosed with frontotemporal dementia in 2022. His wife, Emma Heming Willis recalled the day when Bruce was diagnosed with the condition and how it made her feel "lost, isolated and afraid." Talkin to PEOPLE, Emma said, Bruce "never connected the dots" that he has been diagnosed with frontotemporal dementia. “I think that's like the blessing and the curse of this, is that he never connected the dots that he had this disease, and I'm really happy about that. I'm really happy that he doesn't know about it,” she shared about Bruce, 70.
Bruce Willis' Diagnosis
"On the day Bruce got his diagnosis, we walked out of the doctor's office with a pamphlet and an empty goodbye. No plan, no guidance, no hope, just shock," she explained in front of a packed auditorium, People reported.
In one instant, the family's future disappeared. The Oscar-winning actor, famous for his quick wit and performances in Die Hard and The Sixth Sense, would be leaving his career behind. Emma found herself thrust into a whole new role of full-time caregiver at the same time.
She continued to explain, "I found myself having to keep my family intact, raise our two small girls, and tend to the man that I love while dealing with an illness I hardly knew anything about."
Emma's emotional candor resonated with hundreds of families who have received similar diagnoses and encouraged her to author a book, The Unexpected Journey, scheduled for publication in September. In Emma's words, "This is the book I hope will assist the next caregiver. It is packed with encouragement, wisdom, and the encouragement necessary to walk this path.
What Is Frontotemporal Dementia?
Frontotemporal dementia is a less prevalent type of dementia that mainly occurs in the frontal and temporal lobes of the brain. It tends to affect behavior, personality, language, and movement more than memory, particularly in its initial stages.
In contrast to Alzheimer's, which generally strikes older individuals, FTD can hit at an earlier age—sometimes as young as 40. The symptoms can range from changes in personality, emotional flatness, or the inability to show empathy to impulsiveness, so it is especially hard for spouses and children to cope.
Emma's case illustrates how abrupt and disrupting this diagnosis can be—not only for the patient but for caregivers as well.
Whereas Bruce Willis' diagnosis hit global headlines, the mental toll taken by Emma, his caregiver, was largely in the background—until she decided to come forward.
Caregiving is a respectable position, but it's also a challenging and thankless one. For those who are caring for loved ones with dementia or other chronic illnesses, the stress of "keeping it all together" can result in a condition called caregiver burnout.
"Caring for someone is the most intimate and demanding work of love," Emma explained, "but when you're not noticed or supported, it begins to undermine your health—mentally and physically."
© 2024 Bennett, Coleman & Company Limited

