- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
Musician Matt Willis Shows How Alcohol and Mental Health Intersect and Why Sobriety Can Rewire the Brain
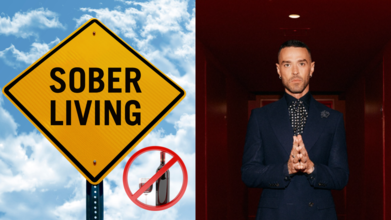
Credits: Canva, mattjwillis/Instagram
Addiction and recovery are rarely straightforward journeys. For many, alcohol does not just affect the body but also deeply intertwines with mental health, shaping how people think, feel, and cope with everyday life. Musician Matt Willis has been candid about how these struggles have shaped his own path.
Willis, the Busted musician who made us all nostalgic for early-2000s pop-punk, has been open about that battle. In a world where Instagram often polishes life until it sparkles unnaturally, Willis recently chose a different route: honesty.
“8 years clean and sober. This week I celebrated 8 years of sobriety. This one feels different. It marks the same length of time I had before my last relapse… and this time I know I’m in a completely different place,” he confessed in a heartfelt Instagram post.
The confession struck a chord because it tapped into something broader: the complex intersection of alcohol and mental health.
Alcohol and the Brain’s Wiring
Alcohol is not just a social lubricant; it is a central nervous system depressant. That means it slows down brain function, interferes with neurotransmitters like serotonin and dopamine, and temporarily boosts feelings of pleasure while causing anxiety and depression once the buzz fades.
For people already navigating mental health challenges, alcohol can act like a short-term plaster on a long-term wound. The relief feels immediate, but the wiring gets fuzzier each time. Over time, the brain starts to rewire itself around those cycles of highs and lows, making it harder to break free.
Willis, who first got sober in 2008 before relapsing and then restarting his recovery in 2017, understands this cycle all too well. “Recovery has to stay front and centre. It might seem selfish when I have a wife and three children, but without sobriety, I lose all of that,” he wrote. That raw honesty underlines a truth experts often echo: recovery is less about restriction and more about survival.
Why does sobriety feel like rewiring the brain?
Neuroscience has an answer. Research suggests that long-term sobriety can actually help the brain rebuild. Neural pathways that once screamed for alcohol begin to quiet down, while new connections linked to healthier coping mechanisms strengthen.Think of it like upgrading your phone’s software after years of ignoring notifications. Suddenly, the glitches ease, the system runs smoother, and your mental health strategies actually work the way they are supposed to.
Matt’s words illustrate this shift. “People sometimes ask if being so open about recovery affects me negatively. Honestly, it’s the opposite. In recovery we pass the message to those still struggling and in doing that, we remind ourselves how far we’ve come… and how close we are to going back if we forget.” That act of sharing is itself part of the rewiring: replacing secrecy and shame with connection and accountability.
What is Recovery?
Recovery is not just about ditching the pint glass. It is about recalibrating how you navigate life’s messiness. For Willis, his wife Emma and his podcast On The Mend play that role. “I wouldn’t be here without some incredible people in my life. My wife, my partner in everything, the good and the bad,” he said, highlighting the importance of relationships in keeping him grounded.
From a health perspective, this support network is crucial. Studies show that people who maintain strong social bonds are more likely to sustain long-term sobriety. The brain, after all, thrives on connection. Oxytocin, the so-called bonding hormone, is as powerful as any chemical found in a bottle of vodka, but without the hangover.
It is Not Just Willis' Story
Willis may be one musician, but his story plays out in countless households, often behind closed doors. Addiction is still wrapped in stigma, especially when entwined with mental health struggles. By speaking openly, he normalises the messy, nonlinear journey of recovery and shows that sobriety is not just about abstinence; it is about rebuilding life from the inside out.
“I don’t often say this, but today I’m really proud of who I am and who I’m becoming. Thank you to everyone who has supported me on this journey so far. I’ve got some big plans for the next couple of years… let’s see how far we can go,” he concluded.
World Hearing Day: Why Ignoring Hearing Loss Can Affect a Child’s Future And an Adult’s Brain

Credits: Canva
Hearing is one of the most vital yet overlooked senses—and its impact extends far beyond the ears. It shapes how a child learns to speak, how a student performs in school, how adults stay socially connected, and even how the brain ages.
As Dr NVK Mohan, ENT and Cochlear Implant Surgeon at CK Birla Hospitals, CMRI, explains, “Hearing is one of the most vital yet overlooked senses, and its impact extends far beyond the ears.”
This World Hearing Day, the focus is clear: ignoring hearing loss doesn’t just affect sound—it affects development, confidence, learning, and long-term brain health.
What Is Hearing Loss?
Hearing loss can happen when any part of the ear is not working in the usual way. This includes:
- The outer ear
- The middle ear
- The inner ear
- The hearing (acoustic) nerve
- The auditory system in the brain
When sound cannot travel properly through these structures—or when the brain cannot process sound clearly—hearing becomes impaired. It may be partial or complete, temporary or permanent, and can occur at any stage of life, from before birth to adulthood.
In Children: The Impact Goes Beyond the Ears
In children, hearing plays a central role in speech and language development. Even mild hearing loss can cause a child to miss critical sounds needed to build vocabulary and clear speech.
Dr Mohan notes, “In children, undetected hearing loss can interfere with speech development, learning ability, and social interaction, often affecting confidence and academic performance well into adulthood.”
Many parents assume that if a child responds to loud sounds, their hearing must be normal. But hearing is more complex than that.
“Healthy hearing requires the ability to perceive sounds across all frequencies, especially those essential for speech and language development,” he explains. “Delayed identification can mean missed developmental milestones that are difficult to recover later.”
Signs of Hearing Loss in Babies
Even if a baby has previously passed a hearing screening, parents should continue to look for warning signs:
- Does not startle at loud noises
- Does not turn to the source of a sound after 6 months of age
- Does not say single words like “mama” or “dada” by 1 year
- Turns head when seeing you but not when you call their name
- Seems to hear some sounds but not others
What may look like inattention can sometimes be partial or complete hearing loss.
Signs of Hearing Loss in Children
As children grow, signs may include:
- Delayed speech
- Unclear speech
- Difficulty following directions
- Frequently saying “Huh?”
- Turning the TV or radio volume up too high
Babies and children are expected to reach developmental milestones in how they play, learn, communicate, and behave. A delay in these areas could indicate hearing loss or another developmental concern—and should prompt a hearing evaluation.
What Causes Hearing Loss?
Hearing loss can occur at any time during life.
Genetic Causes
About 1 in 2 cases of hearing loss in babies are due to genetic factors. Some babies may have family members with hearing loss. Around 1 in 3 babies with genetic hearing loss have a syndrome, meaning they have additional conditions such as Down syndrome or Usher syndrome.
Other Risk Factors
Around 1 in 4 cases are linked to:
- Maternal infections during pregnancy
- Complications after birth
- Spending 5 days or more in a neonatal intensive care unit (NICU)
- Severe jaundice requiring blood transfusion
- Structural differences in the head, face, or ears
- Neurological disorders
- Meningitis
- Severe head injuries requiring hospitalization
Recognizing these risks allows for closer monitoring and earlier diagnosis.
In Adults: When Hearing Loss Affects the Brain
The consequences of untreated hearing loss do not stop in childhood. In adults and older individuals, the risks shift from speech delays to brain health.
Dr Mohan highlights, “In adults and the elderly, untreated hearing loss is increasingly being linked to social withdrawal, memory problems, and cognitive decline.”
When the brain does not receive clear sound input, it must work harder to interpret speech.
“When the brain is deprived of clear sound input, it has to work harder to interpret speech, diverting cognitive resources away from memory and higher mental functions,” he explains. “Over time, this reduced auditory stimulation and social disengagement can increase the risk of accelerated cognitive ageing.”
In simple terms, when hearing decreases, conversations become exhausting. People may begin to withdraw socially. The brain receives less stimulation. Over time, this combination can affect cognitive resilience.
Hearing health, therefore, is closely linked to brain health.
Prevention: What Can Be Done?
While not all hearing loss can be prevented, certain measures reduce risk:
- Maintain a healthy pregnancy
- Ensure children receive recommended vaccinations
- Protect children from high noise levels
- Seek prompt treatment for ear infections
Noise-induced hearing loss, in particular, is preventable with awareness and protection.
Screening and Early Diagnosis: The Most Important Step
The most important message, experts say, is that hearing loss is both detectable and manageable—especially when addressed early.
“Hearing screening is easy and not painful. Babies are often asleep during the test, and it usually takes only a few minutes,” Dr Mohan says.
For Babies
- All babies should undergo hearing screening by 1 month of age.
- If a baby does not pass, a full hearing test should ideally be completed by 3 months.
For Children
- Hearing should be tested before school entry.
- Testing should also be done whenever there are concerns about speech delay, learning difficulties, or recurrent ear infections.
- Routine hearing checks are equally important for adults, particularly as they age.
Why Pap Smear Is Non-Negotiable After 30 And Why So Many Women Still Avoid It | Women's Day Special

Credit: iStock
Vaccinated for human papillomavirus (HPV)? Now, take that Pap smear test. This is the most common advice women hear to prevent the risk of cervical cancer that annually causes around 6,60,000 new cases and around 350,000 deaths worldwide.
However, it's easier said than done for most of the fairer sex.
A Pap smear is typically a gynecological examination where a speculum is inserted to collect cells from the cervix.
Although the procedure is brief and generally safe, the discomfort discourages many from getting screened. Fear of pain, anxiety of the results, form the common psychological barriers worldwide, and is followed by shame, cultural attitudes, and concerns with male clinicians.
A study in Iran, published in the BMJ Open journal in January 2024, showed that psychological stress, cultural issues, and fear, along with limited information and health services, were the biggest hindrances to getting Pap tests.
Another research published in the BMC Women's Health in December 2022, focusing on Africa, Asia, and South America, reported that many women avoided or delayed Pap smears because they are afraid the procedure will hurt. Many also reported being embarrassed about the pelvic exam or fear of having a stranger see their private areas. Some also worried that the test could damage the uterus.
A Pap Smear test, however, is proven to be safe and is recommended for every woman above the age of 21 years.
“A Pap smear is a rapid, safe, and painless screening procedure that detects irregular cellular changes well before they become malignant. The ability to treat at this pre-cancerous stage of disease provides an excellent outcome,” Dr. Tirathram Kaushik, Senior Consultant GI, HPB, Gastrointestinal & Thoracic Oncology and Robotic Surgery, HCG Cancer Centre, Borivali, told HealthandMe.
A 2025 study, published in the Journal of Contemporary Clinical Practice, showed that pap smears are excellent at ruling out precancerous risks. It also remains a valuable screening tool where molecular testing is limited.
There are many myths about Pap smears that make people anxious or avoid screening. Let’s clear up the most common ones:
Pap Smears Are Painful
The most common myth regarding pap smear screening is that it is painful, unnecessary, or only required when symptoms are present.The Pap smear procedure, which takes only a few minutes, is often described as uncomfortable. While some feel like a quick pinch, others experience slight discomfort or spotting. Severe pain is not considered normal.
“From an oncology perspective, this myth results in a delay in diagnosis. Cervical cancer often occurs silently in its early stages, without any noticeable symptoms,” Kaushik said.
I Am Healthy, So I don’t need A Pap Smear
Some people believe that if they feel healthy, they don’t need a Pap smear. However, HPV can cause early cervical cell changes, which usually produce no symptoms.While individuals may feel completely well, they still have abnormal cells developing silently. As a result, regular Pap smear screening is important because it detects these changes early -- before they turn into cervical cancer.
“The HPV infection and subsequent changes that lead to cervical cancer happen slowly over many years. HPV infection is also very common, and one in two women is likely to get infected. Regular screening by a Pap smear will help to catch infection early before it can convert into cancer,” Dr. Deepak Jha, Chief - Breast Surgery & Sr. Consultant Surgical Oncology, Artemis Hospitals, told HealthandMe.
I Have Only One Partner, So I don’t need Screening
HPV can be transmitted even in monogamous relationships. Your partner may have been exposed to HPV before, and the virus can stay in the body for years without symptoms.“HPV doesn’t need penetrative sex for infection. It can be transferred if there is any contact of bodily fluid. It’s always safe to test and be assured rather than repent later,” Dr. Jha said.
Testing Means Cervical Cancer
Many women worry that testing automatically means cancer, which is not true. Screening is preventive, and most results are normal.“Even if HPV is detected, it usually indicates a pre-cancerous stage that is highly treatable,” Dr. Parminder Kaur, Consultant Gynecologic Oncologist at CK Birla Hospital, Delhi, told HealthandMe.
Moreover, a Pap smear only screens for cervical cancer; it can’t detect other gynecological cancers such as cervical, ovarian, uterine (endometrial), vaginal, and vulvar cancers. So, screening and appropriate tests for those will be required, irrespective of the Pap smear.
I Am old, So I don’t need A Pap Smear
HPV infection happens at an early age, so merely old age is not enough to stop Pap smear. At least three consecutive negative screens (minimum three-yearly Pap smears or five-yearly HPV screens) would be needed in this situation.I Got Vaccinated, So I Do Not Need A Pap Smear
The vaccine covers the major variants of the HPV virus, but there is still a small probability of cervical cancer due to the uncommon HPV variants.Irrespective of vaccinated status, a woman should go for regular screening between the ages of 25 and 79. Also, if a woman already had HPV exposure before being vaccinated, she would not benefit, the experts said.
“Screening is not just a routine procedure - it is a preventive measure. In the treatment of cancer, early detection alters the disease course, whereas waiting for symptoms to develop means the disease is likely to be already advanced,” Dr. Kaushik said.
Dr Kaur called for more awareness and stated that open discussion are key to help more women take the important screening test.
When To Get Screened
The United States Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS) recommend getting your first Pap test at age 21, followed by Pap testing every 3 years. Even if you are sexually active, you do not need a Pap test before age 21.
- Individuals must start getting Pap tests at age 21. If the result is normal, repeat the test after three years.
- For individuals aged between 30 and 65 years old, doctors are likely to recommend an HPV test along with a Pap test. If both are normal, repeat after five years.
In women older than 65, you don't need to be screened anymore if:
- You have had at least three Pap tests or two HPV tests in the past 10 years, and the test results were normal or negative, and
- You have not had a cervical precancer in the past, or
- You have had your cervix removed as part of a total hysterectomy for non-cancerous conditions, like fibroids.
Long Covid Causes Lasting Brain Inflammation And Lung Injury, Reveals Study

Credit: Canva
Are you still experiencing brain fog, fatigue, and mood changes even after years of a mild COVID-19 infection? A new study showed that the SARS-CoV-2 virus, behind the COVID infection, can cause persistent brain inflammation and lung injury, according to a study.
Researchers from Tulane University, in Louisiana, US found that the brain inflammation lasts long even after the virus was no longer detectable.
Their study, published in Frontiers in Immunology, can answer why long COVID often includes neurological symptoms such as brain fog, fatigue, and mood changes.
"Long-term effects on the brain were unique to SARS-CoV-2. That distinction is critical to understanding long COVID," said lead author Dr. Xuebin Qin, professor of microbiology and immunology at the Tulane National Biomedical Research Center. Qin also mentioned "lasting lung injury" among COVID patients.
In a mouse model, the team found that immune cells in the lungs failed to fully stand down and also spiked the buildup of collagen -- a protein associated with scarring.
The changes stiffened lung tissue, making breathing feel more labored -- a possible answer to breathlessness faced by COVID survivors.
Further, the researchers also noted no repair to the injury, suggesting the virus may interfere with the lung's natural healing process.
On the other hand, in the brain, the mice with COVID showed signs of persistent brain inflammation weeks later. The team also reported tiny areas of bleeding.
Conducting a gene expression analysis, the team found ongoing inflammatory signaling and disruption of pathways involved in serotonin and dopamine regulation -- brain functions linked to mood, cognition, and energy levels.
What Is Long COVID?
Long COVID is a collection of symptoms that last three months or longer after your first COVID symptoms. They include fatigue, brain fog, headaches, breathlessness, altered sense of smell or taste, headaches, and more.
While many of the Long conditions remain to be fully recognized, some people have more than one symptom.
mRNA Vaccine Against COVID
As per recent data from the World Health Organization, more than 43,000 new cases have been reported from 61 countries, between January and February.
Vaccination that prevents SARS-CoV-2 infection is the most effective way to prevent long COVID.
Recently, the European Medicines Agency (EMA) recommended a marketing authorisation in the European Union (EU) for mCombriax -- a messenger RNA vaccine for protecting people aged 50 years and older against COVID-19 and seasonal influenza (flu).
Co-infection with the influenza virus and SARS-CoV-2 can result in more severe disease than would occur with either SARS-CoV-2 or influenza virus infection alone.
mCombriax works like other vaccines by preparing the body to defend itself against infection. It contains messenger RNA with instructions for making proteins found on SARS-CoV-2 and the following seasonal influenza viruses: influenza type A-H1N1, influenza type A-H3N2, and influenza type B of the Victoria lineage.
© 2024 Bennett, Coleman & Company Limited

