- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Harsh Parenting In Early Ages Can Lead To Behavioral Issues In Girls

Credits: Canva
A new study published in the journal Psychological Medicine suggests a biological explanation for why harsh parenting in early childhood could lead to behavioral problems, especially among girls. The study is titled Harsh parenting, amygdala functional connectivity changes across childhood, and behavioral problems. The study found that girls who experienced harsh parenting showed a difference in how their brain connections developed over time, especially the amygdala. It is a key region that involves emotions. These brain changes may help explain the link between early parenting experiences and later behavioral issues.
How Was The Study Conducted?
The research used data from the Growing Up in Singapore Towards healthy Outcomes (GUSTO) study, a long-term project tracking children’s development from birth. The researchers analyzed brain scans of children at four points between ages 4.5 and 10.5 years, allowing them to observe changes in brain development over time. This longitudinal approach provided a clearer picture than past studies, which often examined the brain at just one point in time or focused on older children.
READ MORE: Strict Parents Raise Great Liars- The Parenting Mistake You Didn’t See Backfiring
To assess the parenting styles, mothers completed a questionnaire called the Parenting Style & Dimensions Questionnaire - Short Version. This was for those with children around 4.5 years old. The questionnaire measured harsh parenting behaviors, such as physical punishments, verbal hostility and punitive discipline. At 10.5 years of age, the same children's behavioral problems were evaluated through two methods:
- The Chid Behavior Checklist, which measured emotional and behavioral difficulties
- Children's Depression Inventory 2nd Edition, a self-report questionnaire that assesses depressive symptoms.
What Did The Study Find?
The researchers found that harsh parenting in early infancy was linked to externalising behavioural problems, such as aggression and rule-breaking, by the time the children were 10.5. However, there was no clear connection between tight parenting and internalising issues like anxiety or depression. Interestingly, when they examined the data by sex, they discovered that these behavioural repercussions were more prevalent in girls than in boys.
ALSO READ: Woman Discovers She Was 4 Months Pregnant Days After Giving Birth—Doctor Explains How
In terms of brain development, harsh parenting did not correlate with amygdala size. However, it was associated with changes in how the amygdala developed in respect to other areas of the brain, including as the anterior cingulate cortex (ACC), orbital frontal cortex, and dorsolateral prefrontal cortex.
A key finding also noted that girls who experienced harsh parenting shower a faster decline in amygdala-ACC connectivity over time. This was linked to a greater likelihood of externalizing behavior problems. The researchers also suggested that this rapid decrease in connectivity may also reflect in the brin when it comes to adapting to early stress. It also has the potential to make girls more prone to behavioral difficulties later in their lives.
The researchers noted: “The present study provided evidence that harsh parenting in early childhood is prospectively associated with both externalizing behavior and the developmental trajectories of functional connectivity profiles of the amygdala, with some support for sex differences at the behavioral and neurocircuitry levels."
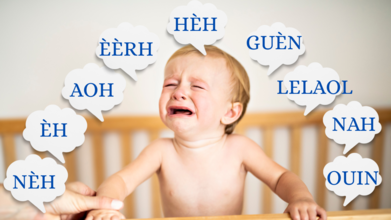
Decoding Baby Cries: What Are They Really Saying?
Credits: Canva
For new parents, a baby’s cry can feel like an unsolvable riddle. Is it hunger, fatigue, discomfort, or something more complex?
While the sound of a crying baby can stir panic and helplessness, researchers say that it’s actually the first language a newborn uses to communicate. Learning to interpret these cries can build trust, reduce frustration, and strengthen the parent-child bond.
The Language of Cries
According to research by Priscilla Dunstan, babies across the world, regardless of culture or language, produce nine distinct sounds in their cries, each indicating a specific need. These are not random wails but physiological reflexes.
For example, when a baby is hungry, the tongue touches the roof of the mouth, creating a “Nèh” sound. Identifying these subtle cues early can prevent discomfort from escalating into distress.
The Nine Cries and What They Mean
Nèh – “I’m hungry”
This sound mimics a sucking motion. It’s usually the first cry parents hear, especially in the early weeks when feeding is frequent.
Èh – “I need to burp”
A short, jerky sound created when air is trapped. If you hear this after feeding, hold the baby upright and pat gently on the back.
Aoh – “I’m sleepy”
This cry often comes with yawns and a wide-open mouth. It signals that your baby needs rest soon.
Éérh – “I have a stomach ache”
Hoarse, prolonged, and strained, this cry is linked to gas or colic. Gentle massage or movement may help soothe your baby.
Héh – “I’m uncomfortable”
A soft 'h' sound may point to issues like a dirty diaper, awkward position, or rash. A quick check can resolve it.
Guèn – “I’m teething”
Often accompanied by drooling and gum rubbing, this sound means your baby may need a teething ring or gentle gum massage.
Lelaol – “I need company”
A softer, almost meowing sound—your baby simply wants interaction. Responding to this helps foster emotional security.
Nah – “I’m thirsty”
A gentler version of the hunger cry, often heard in warmer weather or when breastfeeding intervals increase.
Ouin – “Everything feels wrong”
A full-body cry when a baby is overwhelmed. Cuddling, rocking, or just holding them can bring comfort.
Beyond Sounds: Emotions And Connection
While deciphering these cues helps meet basic needs, it also supports a baby’s emotional growth. Babies experience emotions intensely, and crying is their only outlet. Your calm presence helps regulate their emotional storms, almost like serving as their temporary “prefrontal cortex”, the part of the brain responsible for emotional regulation, which develops later.
Should You Always Respond?
Some parents wonder if responding to every cry will spoil the baby. Experts say that in the early months, every cry deserves attention. It isn’t about temperament, it’s communication. As the baby matures, short self-soothing intervals can be introduced. Still, your consistent presence helps develop secure attachment and emotional resilience.
Breastfeeding Week: Breastfeed, Pumped Milk, Or Formula? Experts Weigh In On What Works The Best For A Mother And Her Child

Credits: Canva
As World Breastfeeding Week brings attention to the nourishment of newborns, the conversation around feeding methods continues to stir debates, and often, guilt. At the heart of it lies a mother’s intent to ensure her baby thrives, yet she is often met with societal pressure to follow a one-size-fits-all approach. Is direct breastfeeding truly superior to pumping? Does choosing formula equate to failure? What about maternal well-being?
To break down these questions, we spoke to Dr. Shailly Sharma, Senior Consultant Gynaecologist at Cloudnine Hospital, Faridabad, and Dr. Anjali Saxena, Senior Dietitian at PSRI Hospital, Delhi.
Breast is Best—but So is Fed
The idea that only direct breastfeeding qualifies as "best" is a common misconception. Dr. Shailly Sharma clears the air.
“The most crucial factor is that the baby receives breast milk. Whether it’s delivered directly at the breast or via a bottle (expressed milk), the nutritional and immune benefits remain largely the same,” she says.
While direct breastfeeding supports jaw development, digestion, and skin-to-skin bonding, Dr. Sharma emphasizes that pumping is an effective alternative, especially for mothers dealing with work demands, fatigue, or medical issues.
Dr. Anjana Saxena adds that, nutritionally speaking, there's only a modest difference, “Freshly expressed milk retains most of its nutrients and immune-protective components. Long storage, especially freezing, may reduce some immune factors like antibodies, but the core nutrients remain intact.”
So whether you breastfeed, pump, or both, the key is ensuring your baby is fed and healthy.
The Invisible Load: Guilt, Shame, and Emotional Toll
New mothers often find themselves navigating an emotional minefield, where breastfeeding is equated with being a ‘good mother’. The guilt of not producing enough milk or having to return to work can take a toll on their physical and mental health.
“Emotional stress, especially self-blame, can significantly affect a mother’s recovery,” explains Dr. Sharma. “It increases cortisol levels, delays healing, disrupts sleep, and may reduce milk supply further. Worse, it can impact bonding with the baby and even trigger postpartum depression.”
She advocates for “compassionate, non-judgmental support” from healthcare providers and society alike.
Dr. Saxena echoes this, “Parenting is not about perfection. When breastfeeding causes stress or health complications, choosing formula can be the healthier option, for both mother and baby.”
Can Formula Ever Compare?
While breast milk contains unique components, live antibodies, enzymes, and human milk oligosaccharides, formula has come a long way in mimicking its nutritional profile.
“Modern infant formulas are designed to closely match breast milk and meet the basic nutritional needs of infants,” says Dr. Saxena. “While they don’t contain certain bioactive compounds, they are a safe and effective alternative.”
She lists bioactives like immunoglobulin A (IgA), lactoferrin, lysozyme, and HMOs, powerful agents in human milk that boost immunity and gut health.
“Formulas today may include prebiotics and DHA, but they still fall short of replicating the dynamic nature of breast milk,” she says, adding, “This doesn’t make formula harmful, it simply means breast milk offers some extra protection.”
Still, when breastfeeding isn’t feasible, formula isn’t a compromise, it’s a responsible, sometimes life-saving, choice.
The Power of Skin-to-Skin Contact
Another overlooked element is the emotional and physiological benefit of skin-to-skin feeding, often linked with direct breastfeeding but equally valuable during bottle-feeding or pumping routines.
“Kangaroo care stabilizes the baby’s temperature and heart rate, reduces stress hormones in both mother and child, and encourages better milk let-down,” explains Dr. Sharma. “Even with expressed milk, incorporating skin-to-skin time is immensely beneficial.”
This helps nurture the parent-child bond, which contributes to overall emotional well-being, regardless of the feeding method.
When Breastfeeding Isn't an Option
Sometimes, no amount of support can overcome low milk supply. And that’s okay, say the experts.
“When a mother cannot produce sufficient milk, supplementing with formula or transitioning entirely is medically acceptable,” says Dr. Sharma. “The priority must always be nourishment and maternal well-being.”
Healthcare professionals play a vital role here. Instead of framing formula as a fallback, they should equip mothers with information on all feeding options, whether that’s formula, donor milk, or continued pumping, free from judgment.
“Mothers need clear guidance, emotional support, and respect for their choices,” she adds.
Ultimately, the debate should never overshadow the reality that every family is different. Feeding journeys can be empowering, exhausting, or even painful. But they are valid, regardless of the route taken.
Dr. Saxena puts it best, “Emotional well-being, mental health, and bonding are just as vital as physical nutrition. Mothers deserve support and compassion, not judgment.”
World Breastfeeding Week: Texas Woman Who Broke Her Own Guinness World Record By Donating 2,645.58 Litres Of Breastmilk

Source: Guinness World Record
In a feat that’s both heartwarming and historic, 36-year-old Alyse Ogletree from Texas has broken her own Guinness World Record by donating an incredible 2,645.58 litres of breastmilk.
Her milk, donated to the Mothers’ Milk Bank in North Texas, has helped save and nourish countless premature babies, many of whom wouldn’t have survived without it. As breastfeeding awareness takes center stage this week, in the month of August, Ogletree’s story brings a renewed focus on the lifesaving value of breastmilk.
Milk of Human Kindness
Alyse, a mother of three, first realized her body produced more milk than her baby needed after her first child, Kyle, was born, 14 years ago. Initially discarding the excess milk, she was introduced to the concept of milk donation by a nurse. That small moment led to a life-altering decision.
Since then, she has made it her mission to help other mothers and fragile infants who cannot access breastmilk. “I have a big heart,” she told the Guinness World Records. “I’m not made of money, and I can’t donate money to every cause. But I can donate what I have plenty of, milk.”
An Impact Measured in Lives
According to the Mothers’ Milk Bank, just one litre of breastmilk can help nourish up to 11 premature newborns. By that math, Ogletree’s contribution could have helped nearly 350,000 babies. Her extraordinary effort is not just a number, it’s a massive public health intervention and a testament to how individual generosity can ripple into nationwide impact.
Breastmilk offers crucial immunity, nutrients, and protection against infections, especially for preemies. For these infants, every drop truly counts.
Balancing Family, Pumping, and Purpose
Ogletree isn’t just a record-breaker, she’s also a full-time mom to Kyle, now 14, Kage (12), and Kory (7), and has even donated milk while serving as a surrogate mother. She credits her consistent donation success to a balanced lifestyle: staying hydrated, eating well, and sticking to a strict pumping schedule.
Despite never being diagnosed with any hormonal condition to explain her overproduction, she believes her body simply found its purpose. “It’s one of the best feelings in the world,” she said. “To know that something my body naturally produces can save lives.”
Beyond setting records, Ogletree is determined to educate and inspire others. She wants mothers to know that breastmilk, even in surplus, should never go to waste, and that donating is easier than many realize.
Her story comes at a critical time. Breastfeeding rates remain inconsistent globally, and many mothers stop early due to lack of support, misinformation, or physical difficulty. Ogletree’s message is simple but powerful: every drop matters, and giving—even a little—can be lifesaving.
As the world observes Breastfeeding Week, Ogletree’s record is more than a headline, it’s a call to action.
© 2024 Bennett, Coleman & Company Limited

