- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
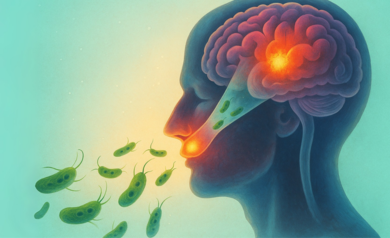
Brain-Eating Amoeba: What To Know About The Microscopic Killer That Took A 12-Year-Old Boy’s Life In Days
Credits: Health and me
Twelve-year-old Jaysen Carr was full of life until a summer day at Lake Murray, South Carolina, changed everything. Days after enjoying the water with his family, he developed symptoms that quickly escalated. Within a week, he was dead.
Doctors confirmed the reason as Naegleria fowleri, a rare and aggressive organism infamously dubbed the “brain-eating amoeba.” The South Carolina Department of Public Health and Prisma Health Richland Hospital in Columbia reported the pediatric death publicly on July 22. It's the first such case in the state since 2016.
The microscopic killer that claimed Jaysen’s life is a naturally occurring amoeba found in warm freshwater. It causes a deadly brain infection called primary amebic meningoencephalitis (PAM), which destroys brain tissue and is almost always fatal.
The Carr family, devastated by their sudden loss, is now seeking answers. Their attorney, Tyler Bailey, stated that while the family appreciates the outpouring of support from their community and the care provided by Prisma Health, they are committed to ensuring such a tragedy doesn't happen to another family.
"They have many questions about how and why Jaysen died," Bailey said in a public statement. “And they want to do everything in their power to make sure this doesn’t happen again.”
What Is a Brain-Eating Amoeba?
Naegleria fowleri is not actually “eating” your brain the way a parasite might devour tissue. But what it does is arguably worse. Once it enters the body—usually through the nose—it migrates to the brain, where it rapidly causes inflammation, swelling, and destruction of brain tissue.
This isn’t something you can catch from drinking water or shaking someone’s hand. It’s not contagious. You have to get water up your nose—typically during activities like swimming or diving in warm, untreated freshwater.
How Common Is Brain-Eating Amoeba?
That’s the strange part, for all its horror, Naegleria fowleri is incredibly rare.According to the CDC, only 167 cases have been reported in the U.S. over the last six decades. And of those, only four people have survived.
Despite this rarity, every summer it resurfaces in headlines because it tends to thrive in the very water bodies people flock to when temperatures rise—lakes, rivers, ponds, and hot springs, especially in Southern and Southwestern states like Texas and Florida.
In Jaysen’s case, the suspected exposure was Lake Murray, although health officials clarified that since the amoeba occurs naturally in many bodies of freshwater, pinpointing the exact source isn’t always possible.
What Causes Brain-Eating Amoeba?
Naegleria fowleri typically infects people when contaminated water enters the nose. Once inside, the amoeba travels along the olfactory nerve into the brain. That’s when things go downhill.
Initial symptoms appear within one to twelve days and may resemble meningitis or flu: headache, fever, nausea, vomiting, stiff neck. But very quickly, the infection escalates to confusion, seizures, hallucinations, coma—and then death. Death usually occurs within 5 to 10 days after symptoms begin.
Where Does Brain Eating Amoeba Come From?
Naegleria fowleri loves heat. It survives in water up to 115°F (46°C), which means late summer is prime time for activity. It’s found in:
- Warm lakes, ponds, and reservoirs
- Hot springs and geothermal waters
- Slow-flowing warm rivers
- Mud puddles and untreated wells
- Poorly maintained swimming pools or water parks
- Untreated municipal water supplies in rare cases
It cannot survive in saltwater, nor in properly chlorinated pools. And again, you can’t get infected by drinking contaminated water—only if it goes up your nose.
How To Avoid Brain-Eating Amoeba?
There is no vaccine or guaranteed treatment for Naegleria fowleri. So prevention is the best—and only—defense. Here’s what health experts suggest:
- Avoid freshwater activities, especially in warm, still water during the summer.
- Hold your nose or use nose clips when swimming or diving in lakes and rivers.
- Avoid stirring up sediment where the amoeba may live.
- Stay away from untreated splash pads and recreational water parks with unclear sanitation practices.
- Never use tap water to rinse your sinuses or fill neti pots unless it’s been properly boiled, distilled, or filtered with a 1-micron filter.
- Even if risk is low, it’s not zero—especially when the result of infection is nearly always fatal.
Why Is Brain-Eating Amoeba So Hard to Treat?
Once symptoms begin, treatment options are limited. The infection progresses too rapidly for most medications to have an effect. Some experimental treatments using antifungal drugs and hypothermia (lowering body temperature to reduce inflammation) have been used in a few survivors. But survival still depends heavily on early diagnosis, which is challenging because early symptoms mimic other common illnesses.
Has There Been Any Survivor Of Brain Eating Amoeba?
In 2024, 14-year-old Afnan Jasim from Kerala, India, stunned doctors by surviving PAM. His case was one of the very few globally where the infection was caught early enough, and an aggressive combination of treatments including antifungal and antibacterial medications, supportive care, and cooling therapies—was able to halt the amoeba’s advance.
Health officials urge calm and reiterate that the risk to the general public is extremely low but for parents, educators, and communities especially those in warmer regions—it’s a time to pay attention.
World First Aid Day 2025: Themes, Importance, And Significance

Credits: Canva
Every second counts in an emergency, and World First Aid Day serves as a timely reminder of the critical role first aid plays in saving lives. Observed annually on the second Saturday of September, this day aims to raise awareness about first aid, encourage training, and empower individuals to respond effectively during crises. In 2025, the day will be observed on September 13th, uniting communities worldwide in their commitment to safety and preparedness.
World First Aid Day 2025 Theme
This year’s theme is “First Aid and Climate Change,” highlighting the need for emergency preparedness in the face of increasingly frequent climate-related disasters. Rising global temperatures, floods, wildfires, and storms are creating new challenges for communities, making first aid knowledge more crucial than ever. The theme underscores that basic first aid is not just for personal emergencies but is essential in building community resilience in a changing world.
Importance of First Aid
First aid can make the difference between life and death in the crucial minutes before professional medical help arrives. Whether it’s cardiac arrest, choking, severe bleeding, or burns, timely action can significantly improve survival chances and recovery outcomes. Equipping individuals with basic first aid skills fosters a culture of preparedness, at home, in workplaces, and in public spaces.
In addition to preventing complications and reducing injury severity, first aid training empowers people to act confidently in emergencies. From performing CPR to controlling bleeding and handling choking incidents, these life-saving skills can transform bystanders into first responders.
Origin and Historical Relevance
The roots of first aid go back to the 19th century when Henry Dunant, founder of the Red Cross, witnessed the suffering of injured soldiers during the Battle of Solferino. This inspired a humanitarian movement to care for the wounded without discrimination. The term “first aid” was later coined by German surgeon Friedrich von Esmarch in the late 1800s.
World First Aid Day was first observed in 2000 by the International Federation of Red Cross and Red Crescent Societies (IFRC) to promote global first aid education. Today, millions of people participate in awareness events, training workshops, and community demonstrations, spreading the message that first aid is a universal skill everyone should learn.
How to Participate
Individuals can get involved by attending first aid training courses, sharing educational resources on social media, organizing community workshops, or volunteering with local Red Cross and Red Crescent societies. Even downloading a first aid mobile app can be a step toward being prepared.
A Step Toward Safer Communities
World First Aid Day 2025 is more than a date on the calendar, it’s a call to action. By learning first aid, we can build safer, more resilient communities ready to face emergencies, including those amplified by climate change. This September 13th, take the time to learn, teach, and spread awareness. You might just save a life.
Non-Communicable Diseases Driving More Deaths in India With Women Facing Highest Risk, Says Lancet Report

Credits: iStock
While most of the world is experiencing fewer deaths from chronic disease, India is heading in the opposite direction. The Lancet's latest analysis reveals non-communicable disease such as diabetes, cancer, and heart disease are shortening more lives—particularly among women. The statistics don't simply provide data, they tell a tale of lifestyle changes, unequal healthcare access, and who bears the largest burden.
A recent paper in The Lancet has shed new light on a disconcerting Indian trend: deaths due to non-communicable diseases (NCDs) are increasing, even as the remainder of the globe experiences improvement. These results indicate a pressing public health threat, with women shouldering the highest burden.
During 2010-2019, the majority of the globe experienced a decline in deaths due to long-term conditions like heart disease, diabetes, and some cancers. Indeed, about 80 percent of nations witnessed a fall, enhancing survival for millions. But India defied this. The research monitored 185 nations and determined that deaths from NCDs went down globally, but India saw a dramatic rise.
For men, the probability of dying from an NCD between birth and age 80 rose from 56 percent in 2001 to nearly 58 percent in 2019. For women, the picture was starker. After a modest decline between 2001 and 2010, mortality rates surged in the following decade. By 2019, the likelihood of an Indian woman dying from an NCD before turning 80 was 48.7 percent, compared to 46.7 percent in 2001.
Why Women Are at Higher Risk?
Whereas men gained advantages in the case of some disease categories like chronic obstructive pulmonary disease (COPD), heart disease, and cirrhosis of the liver, women did not experience gains in most of these categories. Apart from marginal increases in COPD, cirrhosis, and remaining NCD categories, women's mortality risks deteriorated across the board. This indicates increasing gender inequality in access to healthcare, screening, and treatment.
What Are Non-Communicable Diseases?
NCDs, also referred to as chronic diseases, are chronic conditions that unfold gradually. They consist of cardiovascular diseases (heart disease and strokes), cancers, chronic lung diseases such as COPD and asthma, diabetes, and neuropsychiatric diseases. NCDs, as reported by the World Health Organization (WHO), are responsible for 71 percent of total deaths globally. Remarkably, almost three-quarters of premature NCD deaths—deaths that occur before the age of 70—occur in low- and middle-income nations such as India.
The Alarming Case of Lung Cancer in India
A specific trend in lung cancer was emphasized by the Lancet report. Worldwide, lung cancer death decreased among men in 92 percent of nations. But India, Armenia, Iran, Egypt, and Papua New Guinea followed the opposite trend. This highlights India's peculiar susceptibility to lifestyle influences like excess tobacco use, air pollution, and late diagnosis.
Globally, lower deaths due to cardiovascular diseases and certain cancers led to most of the reduction in NCD mortality. However, this achievement was countered by increasing deaths from dementia, liver and pancreatic cancers, and alcohol use disorders. According to the study, although clinical advances such as improved diabetes and hypertension medication, cancer screening, and better emergency treatment of heart attack saved many countries, not all populations were equally exposed.
Why India Is Trailing Behind from the World?
Various structural issues seem to account for India's deteriorating performance. The report cited that the health data quality from India is "very low," which made it more difficult to monitor, prevent, and treat NCDs properly. Meanwhile, disparities in access to medicines, screenings, and preventive care continue to be widespread.
This was also fueled by the 2008 global recession. Its long shadow cut short health budgets and global health aid. Growing poverty, employment insecurity, and inadequate access to healthy foods also intensified inequalities in health. The poor, as well as vulnerable populations—usually women, the old, and poorer communities—were disproportionately hit.
Risk Factors Fueling NCDs
NCDs are highly interrelated with environmental and lifestyle determinants. They are largely driven by tobacco smoking, alcohol consumption, unhealthy diet, and physical inactivity. In India, these are added to by urbanization, air pollution, and unequal access to health care. Social determinants of health, where individuals are born, live, and work, further determine their exposure to the risk factors.
Experts say that it will take systemic transformation to turn around India's NCD burden. Majid Ezzati, lead author of the study and professor at Imperial College London, urged huge investments in healthcare infrastructure, along with tobacco and alcohol control campaigns. These interventions, already proved effective elsewhere in the world, could save millions of lives if successfully adopted in India.
The Lancet report gives a straightforward message: while large parts of the world are set to limit premature deaths from non-communicable diseases, India is in danger of being left behind. Women are especially hit with overly high risks that reflect underlying social and health inequalities.
It will take a two-pronged response—better short-term access to NCD treatments and addressing upstream determinants such as tobacco smoking, unhealthy diets, and air pollution. It also calls for improved monitoring and improved healthcare systems to ensure all groups of people enjoy the benefits.
Scientists Behind Life-Changing Cystic Fibrosis Treatment That Extends Life By Decades Win Medical ‘Nobel’ Prize
Three scientists whose groundbreaking work redefined the future of cystic fibrosis (CF) care have been awarded one of the world’s most prestigious honors in medicine: the Lasker-DeBakey Clinical Medical Research Award. Often referred to as the “American Nobel,” the award recognizes contributions that radically improve human health. This year, it went to Dr. Michael Welsh of the University of Iowa, Paul Negulescu of Vertex Pharmaceuticals, and Jesús (Tito) González, now of Integro Theranostics.
Together, their decades of research led to the creation of Trikafta, a therapy that has extended the lifespan of cystic fibrosis patients by decades and fundamentally reshaped what it means to live with the disease.
When cystic fibrosis was first described in the 1930s, it was considered a fatal childhood condition. Patients rarely survived past elementary school. Even as late as the 2010s, before Trikafta’s approval in 2019, half of patients with CF died before the age of 40.
Today, the outlook is dramatically different. Children born with CF between 2020 and 2024 who have access to Trikafta now face a median survival age of 65 years — nearly indistinguishable from the general population.
As Dr. Eric Sorscher of Emory University explained in The New England Journal of Medicine, “Available projections suggest that health and longevity may increase further as modulators begin to be administered at younger ages.”
This shift marks one of the most profound turnarounds in modern medicine.
The Role of the CFTR Gene
Cystic fibrosis is caused by mutations in a single gene: CFTR (cystic fibrosis transmembrane conductance regulator). The gene is critical for regulating the movement of ions across cell membranes, which in turn ensures proper water balance in tissues.
In healthy cells, CFTR forms channels that allow ions to flow freely. But in CF, the mutated gene produces faulty channels. The result is thick, sticky mucus that clogs the lungs and digestive system, fuels recurrent infections, and damages organs over time.
Dr. Michael Welsh, a pulmonologist and molecular biologist, helped illuminate the exact ways the most common CF mutation, delta-F508, disrupts cell function. He discovered two problems: the defective protein often gets “trapped” inside cells before reaching the surface, and even when it does reach the surface, it underperforms.
In a pivotal experiment, Welsh showed that simply lowering the temperature of cells allowed the trapped protein to move correctly. “That meant it was not totally broken,” he later recalled — a crucial realization that opened the door to correcting the defect.
Meanwhile, as a postdoctoral researcher in Nobel laureate Roger Tsien’s lab, Jesús (Tito) González developed a real-time system to track ion movement across membranes. Initially designed to study neurons, this tool proved invaluable for testing whether new drugs could restore CFTR function.
Negulescu and the Push to Find a Therapy
At Vertex Pharmaceuticals, Paul Negulescu helped drive the systematic search for compounds that could repair CFTR defects. Guided by Welsh’s molecular insights and González’s imaging system, the team screened thousands of molecules. The result was Trikafta, a triple-drug therapy that addressed the underlying cause of CF for most patients.
'Trikafta' Of Game-Changer in CF Treatment
Approved by the FDA in 2019, Trikafta combines three drugs — elexacaftor, tezacaftor, and ivacaftor — that work synergistically to help defective CFTR proteins fold correctly, reach the cell surface, and function effectively. The impact has been extraordinary. Since its introduction:
- Hospitalizations for lung infections have plummeted.
- The need for lung transplants has declined.
- Patients report stronger lung function, weight gain, and dramatically improved quality of life.
- For many families, the treatment has meant that milestones once unimaginable — graduating college, starting families, living into retirement — are now within reach.
Recognition at the “American Nobels”
The Lasker Awards, founded in 1945, celebrate biomedical achievements that shape the future of health. They are considered one of the highest honors in science, often predicting future Nobel Prizes.
The recognition of Welsh, González, and Negulescu underscores the profound impact of their work. The $250,000 prize, while symbolic compared to the billions Trikafta has generated, highlights the ethical and humanitarian dimension of their achievement: turning a once uniformly fatal disease into a chronic, manageable condition.
What CF Treatment Means for Medicine?
The CF breakthrough is not just about one disease. It represents a paradigm shift in genetic medicine. By targeting the root molecular defect rather than simply managing symptoms, Trikafta has become a model for other genetic conditions, from sickle cell disease to rare metabolic disorders.
It also illustrates the power of partnerships between academic researchers, biotech innovators, and patient foundations. The Cystic Fibrosis Foundation’s early investments in research were critical to advancing the work that ultimately led to Trikafta’s approval.
While Trikafta has transformed care in wealthy countries, challenges remain. The therapy is expensive — with an annual price tag of over $300,000 in the U.S. — putting it out of reach for many patients globally.
Furthermore, a subset of CF patients with rare genetic mutations still do not benefit from the drug, leaving an urgent need for alternative therapies. And as with all long-term treatments, researchers must continue monitoring for side effects and resistance.
Roughly 100,000 people worldwide live with cystic fibrosis. For decades, their lives were defined by daily medical regimens, frequent hospitalizations, and shortened lifespans. Today, thanks to the pioneering work of Welsh, González, and Negulescu, those same patients are looking toward futures filled with possibility.
© 2024 Bennett, Coleman & Company Limited

