- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
Know All About The Candidozyma Auris, The Fungal Pathogen And A Rising Health Threat
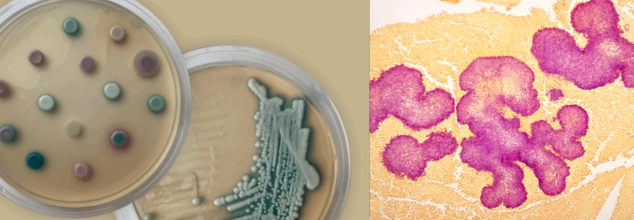
Credits: UKHSA & Canva
As the world is struggling with the rising COVID-19 cases, another global health threat may be lingering, notes UK Health Security Agency (UKHSA), it is the Candidozyma auris.
It is a recently discovered fundus, notes the UKHSA, and is a type of microorganism, which can make you ill. We are often surrounded by fungi, but do not realise it. However, there may be some kind which could pose significant health threats and can also spread silently, even in hospitals. This is Candidozyma auris, or the C. auris, which was formerly known as Candida auris.
C. auris rarely causes infections in healthy people but can be dangerous for those in hospitals—especially patients who are critically ill, have been admitted for long periods, or have weakened immune systems. First discovered in 2009 in a patient’s ear in Japan, it has since spread to over 40 countries across six continents. What makes C. auris particularly worrisome is its ability to survive on surfaces for extended periods, including in hospital settings, and its resistance to many commonly used treatments and disinfectants.
How Does It Spread?
C. auris mainly spreads through contact with contaminated surfaces, medical equipment, or directly from people who carry the fungus. Some individuals may have C. auris on their skin without showing symptoms—this is called colonisation. However, if the fungus enters the body through a wound or medical device like a catheter or drip, it can lead to infection.
In healthcare settings, C. auris can easily pass from one person to another. Colonisation can happen simply by touching surfaces or items that carry the fungus. It has been found on various hospital objects, including bedside equipment, radiators, sinks, windowsills, and medical tools such as thermometers, blood pressure cuffs, and stethoscopes.
What Are The Illnesses Caused By C. auris?
C. auris infections can vary in severity. Some people may carry the fungus without any symptoms, while others can develop serious infections in the blood, brain, spinal cord, bones, abdomen, wounds, ears, lungs, or urinary tract. Even those without symptoms can still develop an infection later or spread the fungus to others.
Who is at risk?
C. auris mainly affects people in hospitals or other healthcare settings, particularly those with weakened immune systems. This includes:
- Patients who have received medical care abroad in the past year, especially from countries with ongoing C. auris outbreaks
- Individuals with long hospital stays
- Patients using medical devices that go inside the body (like catheters or IV lines)
- People in intensive care units
- Those who have taken certain antibiotics previously
- People who are colonised (carrying the fungus without symptoms) can do so for months or even years, putting them at ongoing risk of infection and making it easier for the fungus to spread to others.
Could These Common Cancer Drugs Could Be The Key To Reversing And Treating Alzheimer’s?
Credits: Canva
Alzheimer’s has long been one of medicine’s most frustrating puzzles. Despite decades of research and billions in funding, we still don’t have a cure, and the handful of approved treatments offer only modest relief. But now, scientists from UC San Francisco and the Gladstone Institutes may have uncovered an unlikely lead: two cancer drugs that could potentially reverse Alzheimer’s-related brain changes.
The findings, published in the journal Cell, are generating buzz for one big reason: they didn’t come from years of trial-and-error drug development, but from a computational deep dive into big data, gene expression, and real-world patient records. The research team didn’t set out to find a miracle—yet what they discovered might just change the way we treat one of the world’s most devastating neurological diseases.
To understand how this started, let’s zoom in on what actually happens in the Alzheimer’s brain.
In people with the disease, neurons and glial cells undergo dramatic shifts in gene expression—the biological instructions that tell a cell how to function. These changes disrupt memory, cognition, and eventually basic bodily functions.
Instead of targeting a single protein (like beta-amyloid plaques, the long-standing focus in Alzheimer’s research), UCSF scientists took a broader approach. They analyzed single-cell gene expression data from brain tissue donated by individuals with and without Alzheimer’s. This allowed them to pinpoint the exact genetic changes happening in both neurons and glia during disease progression.
Then came the twist: they used a database known as the Connectivity Map—essentially a chemical encyclopedia—to match those Alzheimer’s gene expression patterns against thousands of existing drugs. The goal? To find drugs that reverse those patterns.
Out of 1,300 drugs studied, 86 had the potential to reverse Alzheimer’s-associated gene changes in at least one brain cell type. Only 25 affected multiple cell types. And of those, just 10 were already FDA-approved.
That’s how two unexpected candidates—letrozole (a breast cancer drug) and irinotecan (used for colon and lung cancers)—emerged as frontrunners.
The team didn’t stop at computer modeling. They turned to electronic health records, combing through anonymized data from 1.4 million patients over the age of 65 in the UC Health Data Warehouse.
What they found was striking: patients treated with letrozole or irinotecan had lower rates of Alzheimer’s. This wasn’t a controlled trial, but it was a strong signal—and one worth testing further.
So the team brought the drugs into the lab, using mice genetically engineered to develop Alzheimer’s-like symptoms. As the mice aged and memory declined, the researchers treated them with each drug, individually and in combination.
The drug combo not only reversed the abnormal gene expression signatures—it also reduced brain degeneration, lowered toxic protein buildup, and restored memory in the mice.
“It’s incredibly encouraging to see the validation of computational predictions in a rigorous animal model,” said Dr. Yadong Huang, senior investigator at Gladstone and co-senior author of the study. “This points toward a real path forward.”
Why Repurposing Drugs Is a Game-Changer?
Developing new drugs from scratch is notoriously slow, risky, and expensive. On average, it takes over a decade and billions of dollars to bring a new drug to market. Alzheimer’s drugs, in particular, have a poor track record. Many promising candidates have failed in late-stage trials, often because they target a single mechanism in a disease that’s anything but simple.
Repurposing existing drugs changes that calculus. “These are already FDA-approved,” said Dr. Marina Sirota, co-senior author and interim director of UCSF’s Bakar Computational Health Sciences Institute. “We’re not starting from zero. We know their safety profiles, which speeds up the timeline dramatically.”
Instead of 10 years, researchers believe this approach could move into clinical trials within two or three.
How Might These Cancer Drugs Work Against Alzheimer’s?
It’s still early, but there are theories. Letrozole is known to suppress estrogen, a hormone that regulates a wide network of genes, including those involved in cognition and brain metabolism. Estrogen suppression might realign gene expression in neurons affected by Alzheimer’s.
Irinotecan, on the other hand, may dampen inflammation by limiting the proliferation of glial cells. In Alzheimer’s, glia often overreact, causing harmful inflammation that contributes to neurodegeneration.
Other hypotheses suggest these drugs may improve how brain cells use energy—a process that often breaks down in neurodegenerative diseases.
Still, researchers caution that what works in mice doesn’t always translate to humans.
What About the Side Effects?
This is where the optimism meets reality. Both letrozole and irinotecan come with known and serious side effects. Letrozole can cause hot flashes, joint pain, and fatigue. Irinotecan’s side effects can include severe diarrhea, nausea, and immune suppression.
“These are potent medications designed to fight cancer,” Dr. Huang noted. “We’ll need to carefully assess whether their risks are acceptable for Alzheimer’s patients, especially in earlier stages of the disease.”
There’s also the question of dosage. Researchers may be able to use lower, safer doses when the drugs are repurposed—something future clinical trials will explore.
So, what’s next? The team is already planning a clinical trial to test the drug combination in people with Alzheimer’s. If successful, this would be the first time a repurposed cancer therapy was proven to meaningfully reverse cognitive decline in humans.
But even if these drugs don’t turn out to be the answer, the methodology could be.
“This is a new way of looking at neurodegenerative disease,” said Dr. Sirota. “Instead of going after one broken part, we’re looking at the whole system—and using big data to identify tools that are already in our toolbox.”
It’s too early to call this a cure. But in a field desperate for fresh approaches, this study offers something rare: real hope.
Alzheimer’s has resisted every easy fix. But by turning to unexpected sources—like cancer drugs—and using advanced data analysis, researchers may have found a new way forward. It’s not a silver bullet, and it won’t be without challenges. But this is one of the most promising leads in years—and it might just mark the beginning of a new chapter in Alzheimer’s treatment.
FDA Clears Prefilled Syringe for Shingles Vaccine, Aim Is for Smoother Administration

Credits: Canva
In a move that could make the shingles vaccination process smoother for both patients and healthcare providers, the U.S. Food and Drug Administration (FDA) has approved a new prefilled syringe version of Shingrix—the widely used vaccine for shingles, or herpes zoster.
The vaccine, developed by global biopharma company GSK, has already been a go-to option for adults aged 50 and older and certain immunocompromised individuals. With this newly approved version, the process of getting vaccinated becomes significantly simpler, without compromising efficacy or safety.
From Two Vials to One Prefilled Syringe
Until now, Shingrix has been administered in a two-step process. It involved combining two separate vials—a freeze-dried (lyophilized) powder containing the antigen, and a liquid adjuvant, by trained healthcare workers just before the vaccine was given.
This mixing step, while manageable, added a layer of complexity that could sometimes slow down the vaccination process, particularly in busy clinics or pharmacies.
With the FDA’s approval of the prefilled syringe, that extra step is eliminated. The vaccine is now available in a ready-to-use format, making the administration process quicker and reducing the chances of handling errors.
For healthcare professionals, this means less prep time and more streamlined delivery. For patients, it could mean shorter waiting times and potentially increased access.
Who Can Get the New Shingrix Syringe?
The approved prefilled syringe format maintains the same usage guidelines as the original formulation. It is licensed for use in:
- Adults aged 50 years and older
- Adults aged 18 years and older who are or will be at increased risk of shingles due to immunodeficiency or immunosuppressive conditions (from either illness or medical treatments)
This broadened scope ensures that vulnerable individuals, like those undergoing chemotherapy, transplant patients, or people living with HIV, can continue receiving this critical protection against shingles, now in a more efficient form.
Why This Matters
Shingles isn’t rare—in fact, according to the Centers for Disease Control and Prevention (CDC), about 1 in 3 Americans will develop shingles in their lifetime.
It is caused by the reactivation of the varicella-zoster virus, the same virus responsible for chickenpox. When it comes back, often years later, it manifests as a painful rash, often accompanied by burning or shooting pain.
In some cases, it can lead to long-term complications like postherpetic neuralgia, where pain lingers for months or even years after the rash clears.
“This new presentation of Shingrix was developed to streamline the vaccination process, supporting health care professionals to provide protection against shingles,” said Tony Wood, Chief Scientific Officer at GSK, in a statement. “Shingles is a disease that one in three U.S. adults will develop in their lifetime.”
The FDA’s decision was based on data that demonstrated technical comparability between the new prefilled syringe format and the original two-vial version. That means the vaccine’s safety, quality, and effectiveness remain unchanged in the updated version.
Bruce Willis Health Update: A Diagnostic Timeline From Aphasia To Dementia

Credits: Wikimedia Commons
The beloved Die Hard star, Bruce Willis, now 70, is spending his retirement surrounded by close family while navigating the challenges of frontotemporal dementia (FTD), a progressive brain disorder. Willis publicly stepped away from acting in 2022 after being diagnosed with aphasia, a condition that affects the ability to communicate. A year later, his family revealed the underlying cause: FTD, a condition that gradually affects speech, behavior, and cognition.
Today, Willis remains alive and cared for at home, surrounded by his blended family, including wife Emma Heming Willis, ex-wife Demi Moore, and his five daughters. While his public presence has faded, his family's updates keep fans connected to his journey.
From Aphasia to Frontotemporal Dementia
In March 2022, fans were shocked by a family statement revealing Willis had been diagnosed with aphasia. The announcement was brief but clear: the condition was affecting his cognitive abilities and making it impossible for him to continue his acting career. However, aphasia was just one piece of the puzzle.
By February 2023, a more specific diagnosis emerged. The Willis family confirmed Bruce was dealing with frontotemporal dementia, a degenerative condition that often begins with language difficulties and eventually affects decision-making, emotional regulation, and behavior.
"Challenges with communication are just one symptom of the disease Bruce faces," the family shared at the time, emphasizing that the condition affects far more than speech.
Unlike Alzheimer’s disease, FTD tends to strike earlier, often in one’s 50s or 60s—and can progress quickly. It affects the frontal and temporal lobes of the brain, areas associated with language, behavior, and executive function. Currently, there is no cure.
The Emotional Weight of Caregiving
Emma Heming Willis has taken on a leading role in Bruce's care and advocacy. Over the past two years, she’s become a vocal supporter for caregivers and families dealing with dementia.
In a People magazine interview published in May 2025, Emma opened up about the early days of Bruce’s diagnosis. “We received a diagnosis and were sent away with no hope, no guidance, no nothing. I really had to figure out how to put resources into place,” she shared, reflecting the emotional and logistical maze caregivers often face.
Her journey inspired her to create resources and support networks for others in similar situations. She continues to document parts of this experience on social media—not to focus on Bruce’s decline, but to highlight the love, humor, and resilience that continue to exist in their home.
A Strong Network of Caregivers
Demi Moore and Bruce’s daughters, Rumer, Scout, Tallulah, Mabel, and Evelyn—have all rallied around him. Their Instagram tributes are filled with gentle moments: shared hugs, quiet celebrations, and messages of gratitude for their father.
For Bruce’s 70th birthday earlier this year, Demi posted a photo with the caption, “Quality time with our BW,” offering a glimpse into their enduring bond. Similar updates on Father’s Day and family anniversaries have become testaments to togetherness in the face of change.
Rather than leaning into clinical details, the family’s posts focus on presence and love—showing the world how meaningful care can look even during decline.
His final films, including Assassin and Detective Knight: Independence (both released in 2023), were completed amid his health challenges. Retrospectively, fans and critics noted that the simpler roles and shorter production schedules may have been early accommodations to his changing condition.
When his retirement was officially announced on March 30, 2022, daughter Rumer posted:
“To Bruce’s amazing supporters… Bruce has been experiencing some health issues and has recently been diagnosed with aphasia… With much consideration, Bruce is stepping away from the career that has meant so much to him.”
From Celebrity Story to Public Health Conversation
Bruce Willis’ diagnosis has helped bring attention to aphasia and FTD, two conditions that are often misunderstood and under-discussed. His family's openness has inspired conversations around the emotional and practical realities of caregiving, early diagnosis, and the importance of support.
© 2024 Bennett, Coleman & Company Limited

