- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
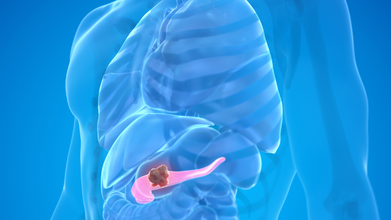
Spanish Scientists Find Breakthrough Cure For Pancreatic Cancer
Credit: Canva
In a breakthrough study, a group of Spanish researchers have created a drug-based cure that can kill pancreatic cancer tumors in the body and eliminate the disease completely.
A study from the Spanish National Cancer Research Centre (CNIO) found that a combination of three drugs, known as CNIO therapy, can shut down multiple tumor survival mechanisms at the same time, preventing the cells from the rewiring themselves and defeating the treatment
Led by renowned cancer biologist Dr Mariano Barbacid, the authors wrote of the results: 'These studies open a way to design new combination therapies that can improve the survival of patients with pancreatic ductal adenocarcinoma. These results set the direction for the development of new clinical trials."
How Does The Drug Work?
To overcome cancer's ability to block the effects of singular therapy drugs, Dr Barbacid’s team attempted attacking the cancerous tumors from three directions together.
The first drug, daraxonrasib, blocked the main KRAS signal that drives tumor growth while the second drug, afatinib, shut down EGFR and HER2, both pathways that cancer cells often use to escape KRAS-targeted treatment.
The third drug, SD36, stopped the functioning of bSTAT3, a backup system that helps cancer cells survive stress and resist therapy.
In the mice study, when scientists combined and used all three drugs together in the rodents, they saw the pancreatic tumours shrank completely and did not return, even more than 200 days after treatment stopped.
The same effect was seen in genetically engineered mouse models and in tumors taken from human patients that were grown in a laboratory. The animals who underwent CNIO therapy did not show serious side effects, suggesting the combination could be safe enough to test in humans.
Despite promising results, the authors advised caution and noted: ""We are not yet in a position to carry out clinical trials with triple therapy. The authors themselves warn that optimising this combination for patients will be a complex process, although they are confident that the finding will set the course for future trials."
Pancreatic Cancer: All You Need To Know
Pancreatic cancer typically begins in the ducts of the organ and can rapidly spread from there to the rest of the organ. Early-stage pancreatic tumors do not show up on imaging tests, making this version of the disease difficult to diagnose until it infects other organs.While there are no clear signs of early pancreatic cancer, symptoms begin to show once the disease reaches the digestive system. Some of these include:
- Jaundice (yellowing of your skin).
- Dark urine
- Light-colored stool
- Upper abdominal pain
- Middle back pain
- Fatigue
- Itchy skin
- Nausea and vomiting
- Gas or bloating
- Lack of appetite
- Blood clots
- Weight loss
- New-onset diabetes
Certain prominent risk factors include smoking cigarettes, cigars and using other forms of tobacco; obesity; Type 2 diabetes and genetic factors.
Pancreatic cancer is also resistant to many common cancer drugs and it notoriously difficult to treat, making this discovery exceptionally important in the search for a permanent cure.
About 22,000 new cases of pancreatic cancer are estimated to occur annually in India out of which nearly 13,000 die from the cause, making it the 24th most common cancer in India.
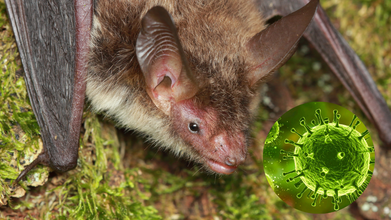
Bird Flu Detected in Dutch Cow, Marking Europe’s First Case

Credit: Canva
Avian or bird flu (H5N1) is a viral infection that spreads in birds, cows and other animals and can cause severe illness and at times, be fatal to humans in rare cases. Until now, the flu primarily affected wild aquatic birds including ducks, geese, gulls and poultry such as chickens as well as turkeys.
However earlier this month, a dairy cow in the Netherlands appears to have been contracted bird flu, making this the first time cattle outside of the United States has suffered the infection.
Previously, transmission of avian flu from cattle to humans has only been reported in the US among farm workers exposed to infected cattle or contaminated environments, and such cases remain sporadic and all developed only mild symptoms.
How Was The Cow Infected?
According to a detailed letter from the Dutch agriculture minister, a cat on a dairy farm in the province of Friesland died from H5N1 last month, which prompted officials to sample blood and milk from cattle at the farm.
Out of the 20 tested, one cow had antibodies to the virus in its milk but did not test positive for the virus itself. “There are also no signs of avian influenza spreading to other dairy farms,” the minister wrote.
The cow had mastitis and respiratory problems last month and its milk was not processed, the letter stated. Also, milk from the farm had been pasteurized, which inactivates the virus and prevents it being transmitted to humans.
“This means that there is very little chance that virus from the infected cow has ended up in the milk for human consumption,” the minister assured. It remains unclear how the virus arrived at the farm or how the cat and cow became infected.
Since October 2025, more than three dozen farms in the Netherlands have had outbreaks and over 1.5 million chickens, turkeys and ducks have been killed to stop the virus’ spread.
Is Bird Flu Dangerous For Humans?
Even though birds are the primary hosts for avian influenza viruses, certain strains can cross species barriers and infect humans and other animals, sometimes causing severe illness.The H5N1 strain drew worldwide concern in the early 2000s because of its high fatality rate in infected people. Although sustained human-to-human transmission is uncommon, infection can occur through close contact with sick or dead birds, their droppings, or contaminated environments.
Bird flu has posed major challenges for both the poultry industry and public health systems, with outbreaks often resulting in large-scale culling to limit the spread.
India has experienced recurring avian influenza outbreaks, particularly in regions with dense poultry farming. Even with strict control measures in birds, the risk of human infection persists, making awareness, hygiene practices, and preventive steps essential for protecting public health.
The common ways humans can contract the virus include:
- Direct contact with infected birds: Handling sick or dead birds, cleaning poultry farms, or working in live bird markets increases the risk
- Exposure to contaminated surfaces: The virus can survive on surfaces such as bird cages, equipment, and clothing. Touching these and then touching the eyes, nose, or mouth can lead to infection
- Consumption of undercooked poultry or eggs: While properly cooked poultry is safe, raw or undercooked meat and eggs from infected birds may pose a risk
- Airborne transmission in poultry farms: In rare cases, workers in enclosed spaces with infected birds may inhale tiny virus-laden particles
RFK Jr. Blames Big Tobacco for America’s Ultra-Processed Food Crisis

Credit: Canva
Robert F. Kennedy Jr. accused Big Tobacco for manufacturing bad, ultra-processed addictive food which has contributed to the country's rising rates of obesity, chronic disease and left many Americans “poisoned”.
In an interview with 77 WABC radio, the Health and Human Secretary claimed that tobacco companies, such as Philip Morris USA, a subsidiary of Altria, had purposely bought food companies and began using scientific techniques to increase consumption in order to escape backlash from cigarette use.
“They saw the regulatory headwinds and litigation headed their way … So, they decided to diversify. And how did they do that? They bought the food companies.
“By 1995, the two biggest food companies in the world were Philip Morris and RJ Reynolds. They moved all of these thousands of scientists who were for years making tobacco more addictive, and they moved them to figure out ways to make food addictive,” RFK Jr. told host John Catsimatidis.
What Did Big Tobacco Do?
The Make America Healthy Again leader explained that the country's major tobacco companies had designed and created foods that were chemically engineered to taste good while offering little to no nutritional value, saying this pattern helped fuel overeating and worsened health.
“They used chemicals and softeners to hijack our brains … The food tastes good. It smells good. But it has no nutrition, so it doesn’t fill you up, so you keep stuffing your pie hole all day. That’s what makes Americans obese.
“It’s not because Americans suddenly got lazy or indolent or hungry,” he added. “It’s because they were poisoned. Their minds were deliberately addicted to eat poison all day long. And we are going to end that now with this administration.”
Tobacco giants such as Philip Morris owns Kraft Foods and General Foods and R.J. Reynolds owns Del Monte Foods and Nabisco. Combined, these companies produce Kraft Macaroni & Cheese, Oreo cookies, Kool-Aid, Jell-O, Hawaiian Punch, Chips Ahoy! cookies, Lunchables, Triscuit and Ritz crackers, Oscar Mayer hot dogs.
Does US Have High Obesity Rates?
Around the same time tobacco companies began to produce fast food food, rates of obesity and the subsequent increased risk for heart disease, stroke and diabetes across age groups jumped across the US.
CDC data from 2017–2020 showed that about 19.7 percent of children and adolescents between ages 2 and 19 had obesity, roughly 14.7 million young people. Among them, 12.7 percent were between ages 2–5, 20.7 percent were 6–11, and 22.2 percent were 12–19.
Dr Vivek Jain, Senior Director & Unit Head, Paediatrics, Fortis Hospital explains that in recent years, obesity among children has risen sharply due to many factors which primarily include unhealthy diets.
READ MORE: Diet, Not Lack Of Exercise Is The Real Reason For Rise In Obesity
While are spending more time in front of screens, getting less outdoor play, and attending online classes, all of which cut down their activity levels. At the same time, fast food, sugary drinks, and packaged snacks have become a regular part of diets.
How To Prevent Childhood Obesity
Prevention needs a joint effort from families, schools, communities, and policymakers. Parents play the most important role, as they shape habits from an early age. Dr. Vivek suggests:
- Balanced nutrition: Encourage home-cooked meals with fruits, vegetables, whole grains, and lean proteins. Limit fried foods, sugary drinks, and packaged snacks.
- Physical activity: Aim for at least 60 minutes of active play or exercise daily, such as sports, cycling, or outdoor games.
- Reduced screen time: Limit television, mobile, and gaming time to help children stay active and sleep better.
- Family involvement: Lead by example—eat meals together, exercise as a family, and make health a priority.
- School initiatives: Schools should provide nutritious meals, promote physical education, and teach healthy habits.
Nipah Virus Outbreak In India: Doctor Says Wider Spread Is Unlikely
Credits: Canva
Nipah virus outbreak in West Bengal has raised concerns across India and in parts of Asia, triggering screenings at airports. India's Ministry of Health clarified on Tuesday that "speculative and incorrect figures regarding Nipah Virus Disease cases are being circulated in certain sections of the media”. This statement was regarding the higher number of cases reported by the media in Kolkata hospital. The statement stressed on the fact that only two cases have been centrally confirmed in West Bengal since December.
Nipah Virus Outbreak India: Can This Infection Become The Next Pandemic?
Many are worried about the Nipah virus outbreak and are speculating whether this could spread to an extent that it could become the next pandemic. Dr T.S. Anish, professor of community medicine and nodal officer for Nipah at the Kerala One Health Centre for Nipah Research and Resilience, as reported by South China Morning Post, said health authorities closely monitor all suspected Nipah cases to make sure no infections are missed. However, he explained that most people who are tested eventually turn out to be negative.
“Out of 100 suspected cases, almost all are usually negative,” he said. He added that tracing every contact of a Nipah patient is difficult, so there is always a chance that a case may appear outside the known contact list. Still, he believes the current outbreak is likely to remain small, affecting fewer than 10 people.
Read: Nipah Virus Outbreak in India, Travelers Screened At Airports
Nipah virus mainly circulates among animals, especially fruit bats, across large parts of Asia. Human outbreaks, however, tend to be limited to specific areas. In South Asia, cases have appeared off and on in Bangladesh and India over the past 20 years, mostly between December and April. Many infections have been linked to people drinking raw date palm sap contaminated by bats.
Kerala has reported Nipah cases occasionally in recent years, including 19 cases in 2019 and six in 2023.
Some medical experts say large outbreaks usually happen only when there are early super-spreader events and continuous person-to-person transmission. That appears unlikely now, as enough time has passed since the cases in West Bengal were identified.
Amir Ullah Khan, professor of health economics at Manipal University, said the timing of the cases raised concern because it coincided with preparations for Lunar New Year travel across Asia. However, he said widespread screening at airports should help prevent the virus from spreading further.
Also Read: Nipah Virus Outbreak In India: All That You Need To Know About This Infection
“If airports continue proper screening, there should not be a major risk of a wider outbreak,” he said, adding that precautions should continue without causing the kind of discomfort passengers experienced during the Covid pandemic.
Nipah Virus Outbreak: Travel Restrictions

After two cases were reported in India's West Bengal, concerns have sparked in many parts of Asia, and measures at airports have been tightened.
- Thailand has begun screening passengers at three airports that handle flights from West Bengal.
- Nepal has also stepped up checks, screening arrivals at Kathmandu airport as well as at several land border crossings with India.
Nipah virus spreads from animals to humans and carries a high fatality rate, estimated to be between 40 percent and 75 per cent. At present, there is no approved vaccine or specific treatment for the infection.
© 2024 Bennett, Coleman & Company Limited

