- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
How Bad Posture At Your Desk Can Trigger Anxiety And Insomnia

Image Credit: Canva
The new work life requires one to chase deadlines, desk jobs and prolonged screen time, which are now the norms, thus, poor posture risk is at its peak than ever. It is because, according to a health specialist, inappropriate sitting positions may bring the impact to humans, as the way people sit can cause not only various physical problems such as headache and neck pain but can also exacerbate mental illness like anxiety and insomnia. A closer look into the issue shows that even such simple matters as sitting posture could provoke serious health problems than one could realize.
Sitting at my desk every day, I never imagined that my posture could impact my well-being. But the headaches, restless nights, and creeping anxiety told a different story. Adjusting my sitting position felt awkward initially, but gradually, I noticed fewer aches and a calmer mind. Small changes truly make a big difference.
Link Between Posture and Mental Well-being
According to the British Heart Foundation, a person spends an average of 66.5 hours per week sitting, which translates into three full days of inactivity. This has seen many spend most of that time seated at desks or in front of screens, and negative effects are becoming apparent from poor posture. In reality, research shows that the majority of people, including twenty-year-olds, suffer from bad posture, which becomes a ripple effect on the body and mind.
Bad postures are not just slouching or sitting crooked. The health issues it can set off are numerous. Medical professionals say that bad postures can cause long periods of tension in the neck and spine muscles. This tension may cause extremely stressful headaches because the constant stress put on the head, neck, and the thoracic spine can sometimes get unbearable. However, poor posture is not solely held responsible for this. Studies found that slouching aids negativity in thinking patterns that can actually impair mood and cause increased stress and sometimes even anxiety and depression.
Maybe the worst consequence of having an improper posture is lack of sleep, known as insomnia. A forward-tilted neck, which is commonly known as "tech neck," can cause muscle fatigue, chronic neck pain, and even difficulty unwinding at night. The tension that builds up in the muscles of the neck and back can make it hard to relax, thus making it harder to fall asleep. This, in turn, contributes to a cycle of poor sleep and heightened stress, which further worsens feelings of anxiety and mental fatigue.
Dangers of "Tech Neck"
Among the many sitting positions that can damage your health, one stands out as being the most harmful: the "tech neck." The head tilts forward when working on screens, which most workers at a desk are familiar with, and also happens for people who spend more hours on their phones. This is because the head appears to weigh much heavier in the neck when the posture is forward. For example, a 30-degree angle can make the head's effective weight go up to 40 pounds and put tremendous stress on the neck and spinal muscles.
This unnatural strain often leads to muscle fatigue and discomfort, which can spiral into chronic neck pain. Over time, this tension doesn't just affect physical comfort; it can trigger persistent headaches and hinder the body's ability to relax, making it more difficult to wind down after a long day of work.
Impact of Prolonged Sitting
The physical consequences of prolonged sitting extend beyond the neck. As humans, our biology was designed to stand and walk. In sitting for long periods of time, the cardiovascular system is disrupted and, therefore, less effective when it comes to the proper functioning of our heart. Sitting also disrupts our digestive system from its norm. The bowel operates better when we are standing up and walking around, a situation not paid much attention to as one sits most of the day.
A sedentary life also contributes to a range of serious health issues, including increased risk factors for cardiovascular disease, diabetes, and even certain kinds of cancer. Over three million deaths are caused globally by physical inactivity worldwide annually. The implications of sitting for too long extend far beyond back pain or stiff muscles; they are related to a whole range of chronic illnesses that can drastically affect the quality of life and even life expectancy.
It is very important to know that posture not only affects the body but can also determine the mental state. According to studies, sitting in a particular way affects cognitive functions and emotional health. For example, slouching in a chair has been said to increase negative thoughts that lead to increased anxiety. However, sitting upright has been proven to promote a more positive attitude that improves mood and self-confidence.
Poor posture can also lead to degradation in cognitive function. Posture can cause shallow breathing leading to low oxygen levels throughout the body and low concentration of oxygen reaching the brain that can impair memory, concentration and overall cognitive performance.
With the advanced use of screens and sedentary work environments, most are unknowingly compromising their mental sharpness by neglecting posture.
How to Sit Best Position
Fortunately, it is easy to improve a posture, which can yield profound effects on the physical health and mental condition. Medical experts recommend "S" posture because gravity is not directed to the spinal muscles. Now, let's see how you do it:
1. Toes and heels flat on the ground: Place your feet flat on the ground such that your knees are kept the same height as that of your hips. As the pressure on your lumbar is reduced, keeping everything in proper alignment as well.
2. Adjust Chair Height: If your chair is too high or too low, your knees may not be at the correct angle, leading to discomfort. Adjust the height of your chair so that your feet rest comfortably on the floor.
3. Back Against the Chair: Ensure that your back is supported by the chair's backrest. If necessary, use a cushion for added support.
4. Refrain from Forward Tilting: Keep your head in neutral, avoiding the forward tilt that leads to "tech neck." This reduces the strain on your neck and spine.
5. Take Frequent Breaks: Even with perfect posture, sitting for long periods can still be harmful. Stand up, stretch, or walk around every 30 minutes to improve circulation and reduce muscle stiffness.
The effect of poor posture goes way beyond mere physical discomfort. It can impact your mental health, your ability to sleep and concentrate, and more. With the increasing hours spent sitting at desks, in front of screens, and on the go, it is more important than ever to pay attention to our sitting habits. Small changes in how we sit can make all the difference in our overall well-being.
We can reduce the risks of headaches, anxiety, insomnia, and chronic pain just by improving our posture and being proactive about reducing sedentary behavior. A healthy posture doesn't only look good; it also feels good, both for your body and mind. So go ahead and adjust your sitting position and give your body and mind the support they deserve to thrive.
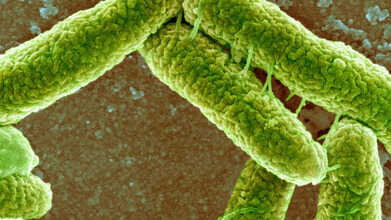
E. Coli Detected In Bhopal Groundwater: Symptoms To Watch And How To Stay Safe
Credits: Canva
Following the water contamination emergency in Indore, similar concerns have now surfaced in Madhya Pradesh’s capital. Groundwater samples collected from four locations in Bhopal have tested positive for E. coli bacteria. In response, the Bhopal Municipal Corporation has barred residents from using groundwater for any purpose.
Officials clarified that the contamination is restricted to underground water sources and has not spread to the treated piped water supplied across the city. According to ANI, civic teams have tested 1,810 water samples so far and inspections are still underway in all zones.
E. coli was the same bacteria responsible for Indore’s recent water crisis, which claimed 20 lives, including that of a five-month-old infant. As per a report by Dainik Bhaskar, fear has gripped several neighbourhoods in Bhopal, with residents hesitant even to touch the water. Locals say the water is unfit not only for drinking but also for washing hands, utensils, or bathing. In some areas, tap water reportedly turns reddish within minutes and emits a strong, foul smell. Adding to the concern, iron levels in the water are said to be nearly 100 times above permissible limits.
Here is what you need to know about E. coli, how it spreads, its symptoms, and ways to stay safe.
What Is E. Coli Bacteria?
Escherichia coli, commonly known as E. coli, refers to a group of bacteria that naturally live in the intestines of humans and animals. Most of these strains are harmless and even play a role in digestion. However, certain types can trigger illness when they enter parts of the body where they do not belong or release harmful toxins.
These disease-causing strains attach themselves to body cells and produce toxins, leading to infection and inflammation.
What Happens During An E. coli Infection?
An E. coli infection occurs when harmful strains of the bacteria enter the body. It most often affects the digestive system, causing symptoms such as watery diarrhoea, abdominal pain, and gastroenteritis. In some cases, the bacteria can also infect the urinary tract.
Certain strains produce Shiga toxin, which can lead to severe complications, including kidney damage, especially in children and older adults.
Why E. coli Infections Occur?
E. coli has many strains. While some support gut health, others can cause serious illness. Experts classify the harmful types based on how they attach to cells and the toxins they release. Several strains are known to cause diarrhoeal diseases, including:
- Shiga toxin-producing E. coli (STEC)
- Enterotoxigenic E. coli (ETEC)
- Enteropathogenic E. coli (EPEC)
- Enteroaggregative E. coli (EAEC)
- Enteroinvasive E. coli (EIEC)
- Diffusely adherent E. coli (DAEC)
Other important strains include uropathogenic E. coli, which is a common cause of urinary tract infections, and E. coli K1, which can lead to meningitis in newborns, according to the Cleveland Clinic.
Common Signs Of E. coli Infection
An infection affecting the gut often begins with digestive symptoms. These may include:
- Diarrhoea that is watery and sometimes blood-stained
- Abdominal pain and cramping
- Reduced appetite
- Mild fever
The Cleveland Clinic notes that watery diarrhoea is usually the earliest symptom when the gastrointestinal tract is involved. Symptoms can vary depending on which part of the body is infected.
How To Protect Yourself From E. Coli?
Preventing E. coli infection largely depends on basic hygiene and safe food practices. Since the bacteria spreads through contaminated food, water, and faecal matter, simple precautions can lower the risk significantly.
Maintain hand hygiene
Wash hands thoroughly with soap and water for at least 20 seconds before eating or cooking, after using the toilet, changing diapers, or handling animals. Proper handwashing removes bacteria and limits its spread.
Practice safe food handling
Use separate cutting boards and utensils for raw meat and ready-to-eat foods. Clean kitchen surfaces and tools with hot, soapy water after each use. Keep raw meat away from fruits and vegetables to avoid cross-contamination.
Cook food completely
Ground meat should be cooked to at least 160°F or 71°C, while poultry needs to reach 165°F or 74°C. Using a food thermometer ensures food is properly cooked and free from harmful bacteria.
Clean fruits and vegetables
Wash all produce under running water just before consumption, even if you plan to peel it. This helps remove bacteria picked up from soil or contaminated irrigation water.
Choose safe drinks
Consume only pasteurised milk and juices, and rely on boiled or treated municipal water. Avoid unpasteurised products and untreated water, as pasteurisation effectively eliminates dangerous E. coli strains.
Childhood Dementia Diagnosis Of A Daughter 'Shattered' Her Father's Life, What Causes This?

Credits: iStock
We often hear of dementia as an adult, or older people's disease, but, a father from Glasgow shares how his four-year-old daughter was diagnosed with the condition. Childhood Dementia news of Darren Scott's daughter was delivered to him like a "complete thunderbolt", he tells Sky News. She was diagnosed with the condition before she turned four. Five doctors were waiting, when Sophia Scott, who had just turned four, were summoned to a Glasgow hospital room. Then came the worst news. Scott was told that his daughter could not live beyond the age of 16. "We were told... there was nothing they could do. It was a moment that broke us, shattered our lives. We have never recovered," he says.
What Is Childhood Dementia?
As per Dementia Australia, childhood dementia is a rare brain condition that affects one in every 2,900 babies globally. Childhood dementia is a group of serious brain conditions that interfere with a child’s memory, behavior, emotions and ability to communicate. It isn’t caused by lifestyle or ageing. Instead, it stems from more than 100 rare genetic disorders that children are born with. These include conditions such as Niemann-Pick type C, Batten disease and Sanfilippo syndrome.
No two children experience childhood dementia in the same way. The illness progresses differently for each child, but one thing remains constant: there is currently no cure. Like adult dementia, childhood dementia is progressive, meaning symptoms worsen over time. Heartbreakingly, around half of all affected children do not survive beyond the age of 10.
What causes childhood dementia?
Childhood dementia is genetic. Globally, about one in every 2,900 babies is born with a condition that can lead to childhood dementia. In Australia alone, an estimated 1,394 children were living with dementia in 2021.
The conditions that cause childhood dementia fall into several categories, including inborn errors of metabolism, lysosomal disorders, mitochondrial disorders, mucopolysaccharidoses, leukodystrophy, neurodegeneration with brain iron accumulation (NBIA), and peroxisomal diseases.
Signs and symptoms to look out for
Symptoms can begin in early childhood or appear much later, sometimes not showing up until the teenage years. The progression may be rapid or unfold slowly over several years, deeply affecting both the child and their family.
Much like adults with dementia, children may struggle with memory loss, confusion, changes in personality, anxiety or fear, and severe sleep disturbances. They may also find it difficult to concentrate, learn, communicate or understand things, and some experience behavioral challenges such as hyperactivity.
In addition, childhood dementia can affect the body beyond the brain. Children may develop problems with their bones or joints, experience issues with the heart, lungs or digestive system, lose their ability to move, see or hear, or have seizures.
As the condition advances, children gradually lose skills they once had — talking, walking, reading, writing and playing. Eventually, the body itself begins to shut down. Without major medical breakthroughs and more research, most children with childhood dementia will continue to face a shortened life, often not surviving beyond their teenage years.
India Faces A Looming Lung Cancer Crisis, Expert Warns

Credits: iStock
India is staring at a sharp rise in lung cancer cases over the next few years, with experts warning that the disease is no longer confined to smokers alone. A recent study published in the Indian Journal of Medical Research projects a significant increase in lung cancer incidence by 2030, with certain regions, particularly the North-East, expected to bear a disproportionate burden. Alarmingly, women are showing one of the fastest rises in new cases.
At a time when the country is on the brink of what researchers describe as a “tsunami” of lung cancer cases, doctors stress that public awareness, early detection, and breaking long-held myths are more important than ever.
Lung Cancer Is No Longer Just a Smoker’s Disease
Lung cancer has long been associated almost exclusively with smoking, but experts say that narrative is outdated. Speaking to The Times of India (TOI), Dr Arun Kumar Goel, Chairman – Surgical Oncology at Andromeda Cancer Hospital, Sonipat, explained that while smoking remains the biggest risk factor, non-smokers are increasingly being diagnosed with the disease.
“Air pollution, indoor cooking smoke, passive smoking, radon gas exposure, occupational hazards like asbestos, and even family history can contribute to lung cancer,” Dr Goel explined. He added that adenocarcinoma, a subtype of lung cancer, is particularly common among non-smokers and appears to be linked more to environmental and genetic factors than tobacco use.
Early Symptoms Are Easy to Miss
One of the biggest challenges with lung cancer is that its early symptoms are often vague and easily mistaken for common respiratory problems. Dr Goel told TOI that persistent cough, changes in cough pattern, coughing up blood or mucus, unexplained chest pain, breathlessness, fatigue, and sudden weight loss are warning signs that should not be ignored.
“In India, lung cancer symptoms often overlap with illnesses like tuberculosis, which leads to delays in diagnosis,” he said. As a result, many patients only seek medical help when the disease has already progressed to an advanced stage.
What a Diagnosis Changes Overnight
A lung cancer diagnosis can be life-altering, both physically and emotionally. According to Dr Goel, patients are suddenly faced with difficult treatment decisions, ranging from surgery and chemotherapy to radiation or targeted therapy. Physical symptoms such as breathlessness and exhaustion can significantly affect daily life.
Emotionally, patients may experience shock, anxiety, fear about the future, concerns for their families, and a loss of independence. “Support from medical teams, counselling services, and loved ones plays a crucial role during this period,” he said.
The Biggest Myth That Delays Care
The most damaging myth, experts say, is the belief that lung cancer only affects smokers. Dr Goel warned that this misconception often results in non-smokers dismissing symptoms or doctors delaying screening. “Anyone can develop lung cancer, regardless of smoking history,” he said.
Early Detection Can Save Lives
If there is one message the public should remember, Dr Goel said, it is that early detection can dramatically improve outcomes. Persistent cough lasting several weeks, unexplained breathing difficulties, or ongoing chest discomfort should prompt immediate medical attention.
“Recognizing symptoms early and seeking help can change the course of treatment and significantly improve quality of life,” he said.
© 2024 Bennett, Coleman & Company Limited

