- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
FOFO (Not FOMO) Is The New Psychological Barrier That’s Fueling a Drop In Health Screenings
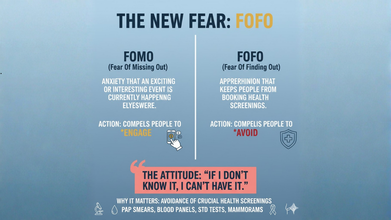
Credits: AI-generated
We all know the feeling of FOMO, the fear of missing out, but there exist another fear, this is FOFO: the fear of finding out. This apprehension is what keeps people from boking their health screenings. The horrors of what will happen after a mammogram, a Pap smear, an STD test, blood panel, or even something as simple as a blood pressure check can scare those with FOFO.
While the term itself is not a medical diagnosis, it is a widely recognized behavioral pattern that both patients and doctors get to see frequently. Over the years, it has gained more attention among experts who deal with health anxiety. As one clinical psychologist explains, there isn’t much published research on FOFO, but practitioners who work with health-related anxiety are very familiar with its impact.
What is even worrying is how common this avoidance has become. As per a 2025 survey of 2,000 employed US adults, 3 out 5 avoid medical screenings altogether, due to fear of bad news or embarrassment. Another 2025 reveal that of 7,000 adults, only 51% attended a routine medical appointment of cancer screening, with a 10% drop from 2024.
The attitude is: "If I don't know it, I can't have it".
Where Does FOFO Come From?
According to psychologists, FOFO often roots itself in anxiety and the desire for control. When something feels uncertain—like a health test result—many people instinctively avoid it. Avoidance becomes a way to quiet the anxiety, at least temporarily.
Experts say FOFO is especially common in people with generalized anxiety disorder, OCD, or illness anxiety disorder. But anyone can experience it. For some, it’s a one-off situation—like hesitating over a prostate exam. For others, it’s part of a broader coping style that involves avoiding anything that feels threatening. Ironically, this sometimes goes hand in hand with endlessly checking symptoms online.
Previous negative experiences in healthcare settings can also feed FOFO. Some people feel anxious around doctors or medical procedures, while others fear being judged, especially when a screening could uncover conditions that carry social stigma—such as STDs. There’s also the fear of receiving results that might force lifestyle changes or treatments they’re not ready for.
A common unspoken belief behind FOFO is:
“If I don’t take the test, then the problem doesn’t exist.”
Waiting for test results adds to the anxiety too. When results take days or weeks, the uncertainty can feel more stressful than the test itself.
How Can You Break The FOFO Cycle?
The first step is by acknowledging what is at stake. Many experts recommend weighing the pros and cons of taking the test versus avoiding it. If FOFO is holding you back, ask yourself what exactly you’re afraid of. Many people underestimate their ability to handle bad news. Understanding this can help reduce the emotional weight of screening.
It’s also helpful to reflect on a few important questions:
- Do I want fear to dictate my health choices?
- What could happen if I keep putting this off?
- A year from now, will I regret not acting today?
These questions often shift the focus from fear to long-term wellbeing. As psychologists note, facing the fear usually leads to decisions that better align with your values.
Norovirus Outbreak In UK: 5 Ways To Protect Yourself From The Vomiting Bug

Credits: Canva
Norovirus appears to be increasing after a 57 percent jump in hospital admissions linked to the sickness bug last week. Figures from the NHS show that an average of 567 hospital beds were occupied each day by patients suffering from diarrhoea and vomiting. Although this number remains well below last winter’s peak, the sudden rise over just one week has raised concerns that norovirus infections could soon climb further.
Experts believe the return of children to school and more indoor contact following the Christmas break may be helping the virus spread.
Why Does Norovirus Spread So Easily?
Jason Murphy, head of pharmacy at Chemist4U, as per The Mirror, said the virus is often underestimated. “Norovirus spreads far more easily than people realise. Even a very small amount can make you ill, and it can stay on surfaces for several days. As cases continue to climb, it’s important to move beyond basic hygiene and take more focused steps to protect yourself and others. Many people think norovirus is a short-lived illness, but it’s very persistent and passes on easily.”
Murphy added that pharmacists tend to approach norovirus from two angles. “We focus on stopping it from spreading and on helping the body cope while the infection passes. There’s no treatment that kills the virus itself, but there are ways to ease symptoms and lower the risk of problems like dehydration.”
Advice To Prevent The Spread Of Norovirus
Treat it as a hard-to-kill infection – Norovirus is classed as a non-enveloped virus, which means alcohol hand gels and many everyday cleaners do not work against it. Washing hands with soap and warm water removes the virus physically, while bleach can neutralise it on surfaces.
Use the right cleaning products – Choose disinfectants that clearly state they are virucidal or effective against non-enveloped viruses. If this is not mentioned, the product is unlikely to kill norovirus.
Get bleach dilution right – Bleach needs to be mixed correctly. If it is too diluted, it will not kill the virus. If it is too strong, it can irritate the skin and lungs. Always ventilate the room well and follow the instructions on the label.
Treat vomiting as contamination – In healthcare settings, vomiting is handled as a form of airborne exposure. Clean beyond the visible mess, air out the space properly, and assume nearby soft furnishings may also be contaminated.
Create isolation at home – If possible, give the unwell person their own bathroom, towels, and bin. This mirrors hospital infection control measures and helps limit the spread to others.
How To Ease Norovirus Symptoms?
Focus on rehydration – Dehydration is the most serious risk linked to norovirus. Electrolyte drinks are more effective than water alone because they replace lost salts as well as fluids.
Take fluids slowly – Sip small amounts every five to ten minutes instead of drinking large volumes at once. This helps reduce vomiting and allows the body to absorb fluids better.
Pain relief – Once fluids are staying down, paracetamol is the safest option for fever, headaches, and muscle aches. Ibuprofen should be avoided if you are dehydrated or vomiting frequently, as it can irritate the stomach and strain the kidneys.
Be careful with anti-diarrhoea medicines – Drugs such as loperamide can slow diarrhoea, but this is not always advised because diarrhoea helps flush the virus out. These medicines may be used briefly in specific situations, such as essential travel, but should not be given to children or used if there is a fever or blood in the stool.
Help with nausea – For severe sickness, a pharmacist can recommend anti-nausea treatments. If vomiting continues, a GP may prescribe medication to help control symptoms so fluids can be kept down.
Eat gently when ready – Once your appetite comes back, start with plain foods like toast, crackers, bananas, or rice. Avoid rich, spicy, or dairy-heavy foods until you feel better.
Rest as part of recovery – The immune system clears norovirus on its own. Getting enough rest supports recovery and helps prevent further complications.
Your Coffee Cup Is Exposing You To Microplastics, Study Suggests

Credit: Canva
The takeaway coffee cup in your hand may be releasing a sea of microplastics into your body every time you take a sip, a new study reveals.
Microplastics are essentially fragments of plastic that are between 1 nanometer and 5 millimetres wide and can found in water, soil and the air. Experts estimate that about 2.7 million tonnes of microplastics seeped into the environment in 2020, an estimate expected to double by 2040.
These fragments carry toxic chemicals and can disrupt internal biological processes, leading to inflammation, cell death, organ dysfunction, heart attacks and reproductive issues in humans. Scientists have also found links between microplastics and cancer.
While researchers have long claimed that microplastics can enter the human body through contaminated food and water, a new Australian study suggests it can also enter through hot coffee cups.
Why Are Plastic Coffee Cups Dangerous?
Based on the Journal of Hazardous Materials: Plastics study, cups made of plastic or with a thin plastic lining can shedding thousands of tiny plastic fragments directly into your drink when filled with hot coffee.Xiangyu Liu, study co-author and research fellow at School of Environment and Science and Australian Rivers Institute, Griffith University, Nathan, said this was due to heat.
The team conducted a a meta-analysis on existing research and analyzed data from 30 peer-reviewed studies. During this time, they focused on how common plastics such as polyethylene and polypropylene behave under different conditions, primarily temperature.
As the temperature of the liquid inside a container increased they noticed that the release of microplastics generally increases too. In the studies reviewed, reported releases ranged from a few hundred particles to more than 8 million particles per litre, depending on the material and study design.
Interestingly, 'soaking time' or the amount of time the drink sits in the cup was not a consistent driver, suggesting that leaving a hot drink in a plastic cup for a long time is not as important as the initial temperature of the liquid when it first hits the plastic.
After testing nearly 400 different cups, they found that if someone drinks '300 millilitres of coffee in a cup made of polyethylene per day, they could ingest 363,000 pieces of microplastic particles every year', according to Liu
What Can Be Done To Reduce Risks?
The team recommends using a reusable cup made of stainless steel, ceramic, or glass, as these materials do not shed microplastics for hot drinks. If you must use a disposable cup, its is better to drink out of a plastic-lined paper cup as they shed fewer particles than pure plastic cups, though neither is microplastic free.
They also advise not pouring putting boiling liquids directly into plastic-lined containers. Telling the barista to make your morning coffee slightly cooler before it hits the cup can reduce the physical stress on the plastic lining and lower overall exposure.
Candida Auris Spreads Across 26 US States; Here’s Who Is Most At Risk

Credits: Canva
A dangerous, drug-resistant fungus has infected more than 7,000 people across 27 US states, including Mississippi, in 2025, federal health data shows. The infection, known as Candida auris, is classified as an “emerging infectious disease,” after doctors and public health experts noted a steady rise in cases since 2019, according to specialists at the Cleveland Clinic.
As of December 20, Mississippi had reported 108 cases of the fungal infection, based on figures from the Centers for Disease Control and Prevention. Here is what you need to know about Candida auris cases in Mississippi.
What Is Candida Auris?
Candida auris is a type of yeast that spreads quickly among patients who are already ill, particularly in hospitals and other healthcare settings, CDC experts say. The fungus can cause a range of infections, from those affecting the skin to severe and potentially fatal bloodstream infections.Treating it is challenging because the organism can adapt to medications meant to eliminate it, health experts note. C. auris mainly affects people with serious underlying health problems and those using invasive medical devices such as ventilators, feeding tubes, or catheters, according to the CDC.
The fungus spreads through contact with contaminated surfaces and objects and can remain on a person’s skin or other body areas even when no symptoms are present. Experts say healthcare workers and visitors are not considered at risk of becoming infected.
Candida Auris: What Are The Symptoms?
Symptoms of Candida auris are not always noticeable, but when they do appear, they may include the following, according to the Cleveland Clinic:
- Ear infections
- Wound infections
- Urinary tract infections
- Blood infections that spread throughout the body
Candida Auris: How Can It Be Prevented?
The CDC advises healthcare facilities to take several steps to limit the spread of Candida auris, including:- Regular hand hygiene using alcohol-based hand sanitizer
- Isolating patients who test positive for C. auris
- Frequent and thorough cleaning of patient rooms
- Using gloves and gowns while providing care
- Ensuring visitors clean their hands with soap and water or alcohol-based sanitizer
Which US States Have Reported Cases Of Candida Auris?
According to CDC data as of December 20, cases have been reported in the following states:
- Pennsylvania
- Illinois
- Indiana
- Michigan
- Ohio
- Wisconsin
- Iowa
- Kansas
- Delaware
- Georgia
- Maryland
- North Carolina
- Virginia
- West Virginia
- Kentucky
- Mississippi
- Tennessee
- Louisiana
- Texas
- Arizona
- Colorado
- Montana
- Nevada
- Utah
- Wyoming
- California
- Oregon
Drug Resistance For Candida Auris Grows
Candida auris, often referred to as a “superbug fungus,” is continuing to spread worldwide and is becoming increasingly resistant to both antifungal drugs and the human immune response, researchers at the Hackensack Meridian Center for Discovery and Innovation said in a review published in early December.
The findings support earlier CDC warnings that labeled C. auris an “urgent antimicrobial threat,” making it the first fungal pathogen to receive that classification, as case numbers have climbed sharply in the United States, especially in hospitals and long-term care facilities.
The review, published in the journal Microbiology and Molecular Biology Reviews, explains why the fungus is so difficult to control and highlights how outdated testing methods and limited treatment options have failed to keep pace. The research was led by Dr. Neeraj Chauhan of Hackensack Meridian CDI in New Jersey, Dr. Anuradha Chowdhary from the University of Delhi’s Medical Mycology Unit, and Dr. Michail Lionakis, head of the clinical mycology program at the National Institutes of Health.
In their statement, reported by Fox News, the researchers emphasized the urgent need to develop new antifungal drugs with broad effectiveness, improve diagnostic tools, and explore immune-based and vaccine-related treatments to better protect high-risk patients.
© 2024 Bennett, Coleman & Company Limited

