- Health Conditions A-Z
- Health & Wellness
- Nutrition
- Fitness
- Health News
- Ayurveda
- Videos
- Medicine A-Z
- Parenting
- Web Stories
WHO Adds GLP-1 Drugs And Cancer Therapies To Updated Essential Medicines List For First Time In 2025

Credits: Canva
The World Health Organization (WHO) has, for the first time, added GLP-1 receptor agonists, popularly known as the active ingredients behind weight loss drugs like Ozempic and Wegovy to its Essential Medicines List (EML). The move, announced Friday, marks a turning point in the global conversation about diabetes, obesity, and equitable access to life-saving treatments.
The Essential Medicines List is one of WHO’s most influential public health tools. Updated every two years, the list identifies medicines that should be available in every functioning health system, regardless of a country’s income level. It now includes 523 medicines for adults and 374 for children. Adoption is widespread: over 150 countries use the EML as a reference point for drug procurement, health insurance coverage, and treatment guidelines.
By including GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy), liraglutide, and tirzepatide (Mounjaro), WHO has formally acknowledged their role not just in diabetes management but also in broader health outcomes, particularly cardiovascular and kidney health.
Also Read: World Physiotherapy Day 2025: Themes, Significance And History
Why the Addition of GLP-1 Drugs is Revolutionary?
GLP-1 receptor agonists mimic a natural hormone that regulates blood sugar and appetite. They stimulate the pancreas to release insulin, slow digestion, reduce liver glucose production, and act on the brain to suppress hunger. This dual benefit—controlling diabetes and supporting weight loss—has propelled them into mainstream awareness.
Scientific evidence reviewed by WHO’s Expert Committee confirmed their ability to lower blood sugar, reduce risks of heart and kidney complications, support weight management, and even extend life expectancy in people with type 2 diabetes and related conditions. For patients with cardiovascular disease, kidney disease, or obesity, these drugs are emerging as game-changers.
The Limits of the Decision
It’s important to note that while GLP-1s are popularly associated with weight loss, WHO stopped short of endorsing them for obesity alone. The drugs were added specifically for adults with type 2 diabetes mellitus who also have established cardiovascular disease, chronic kidney disease, or obesity.
This distinction matters. While obesity affects over one billion people worldwide, WHO’s cautious stance reflects the still-limited long-term data on safety, sustainability of weight loss, and cost-effectiveness in populations without diabetes.
Barriers to Access
Affordability remains the biggest hurdle. Médecins Sans Frontières (MSF) called the decision a “critical milestone” but highlighted that in low-resource settings, GLP-1s are practically out of reach.
A recent MSF study found GLP-1 agonists can cost up to 400 times more than their estimated manufacturing price, while rapid-acting insulin analogues also newly included on the list—are priced 75 times higher than what they could be profitably produced for.
Also Read: Blood Pressure Guidelines Get An Update After 8 Years, Here's All That You Need To Know
“Rapid-acting insulins and GLP-1s are unaffordable and often unavailable in low-resource and humanitarian settings,” said Elizabeth Jarman of MSF’s Access Campaign. “Countries must act quickly to update national EMLs, plan procurement, and push pharmaceutical corporations to make them affordable.”
WHO echoed this call, urging governments to prioritize patients who would benefit most, support generic competition to drive prices down, and ensure distribution at the primary care level, especially in underserved areas.
Expanding the Scope Cancer Treatment
The 2025 update of the EML goes far beyond GLP-1s. Twenty new medicines were added for adults, alongside 15 for children. Notable inclusions are:
Cancer Immunotherapies: Pembrolizumab (Keytruda) and alternatives atezolizumab and cemiplimab for metastatic cervical, colorectal, and non-small cell lung cancers. These immune checkpoint inhibitors have been shown to prolong survival by four to six months in advanced cancers.
Cystic Fibrosis Therapy: Trikafta (a triple-combination drug by Vertex Pharmaceuticals) was hailed as a “historic breakthrough” by patient advocacy groups, marking the first time a cystic fibrosis-specific therapy made the EML.
Insulin Expansion: Short-acting insulin analogues were added, complementing the long-acting formulas already listed since 2021. This creates a complete set of recommended insulin therapies, critical for tailoring diabetes treatment.
Vaccines and Pediatric Medicines: The children’s list now includes drugs for haemophilia, cystic fibrosis, and newly approved vaccines for malaria and mpox.
Tensions Over Excluded Drugs
Not all proposals made it onto the list. Knowledge Ecology International criticized WHO for excluding risdiplam, a treatment for spinal muscular atrophy (SMA). The drug, they argued, is effective, relatively inexpensive to manufacture, and could transform outcomes for children with SMA.
WHO’s Expert Committee deferred inclusion due to incomplete trial data, though subsequent studies published later in the year showed highly promising results.
How Does The Updated Essential Medicine List Affect Global Health?
The stakes of WHO’s decision are high. Diabetes and obesity are among the most pressing health challenges worldwide. More than 800 million people are living with diabetes, half without treatment, while obesity affects over a billion. These conditions are not confined to wealthy nations; their fastest growth is occurring in low- and middle-income countries.
Including GLP-1s in the Essential Medicines List sends a strong signal to governments, insurers, and pharmaceutical companies: these drugs are not luxury treatments for the wealthy but part of the global standard of care.
Yet the path from inclusion to access is not straightforward. Countries must adopt the drugs into their national lists, negotiate prices, and strengthen health systems to deliver them effectively. As David Reddy, director-general of the International Federation of Pharmaceutical Manufacturers, pointed out, inclusion on the list must be accompanied by infrastructure, diagnostics, and trained professionals.
Cancer treatments remain one of the most tightly scrutinized areas of the EML. Cancer kills nearly 10 million people each year, accounting for one in three premature deaths from non-communicable diseases. Despite the flood of new cancer drug approvals in recent years, WHO only recommends therapies that demonstrate clear survival benefits of at least four to six months.
The inclusion of pembrolizumab and its alternatives reflects both clinical evidence and a deliberate effort to reduce global inequities in cancer care. Still, the high cost of immunotherapies poses a major barrier. Without mechanisms like tiered pricing and voluntary licensing, poorer countries may struggle to make these life-extending drugs widely available.
The 2025 Essential Medicines List reflects both optimism and realism. On one hand, it celebrates remarkable advances in science—from GLP-1s reshaping diabetes care to breakthrough therapies for cystic fibrosis and cancer. On the other, it acknowledges the sobering reality of cost and access.
Disposable Face Masks From The Covid-Era Are Turning Into Toxic Microplastics Bombs

Credits: Canva
When COVID-19 ravaged the globe, disposable face masks became a instant necessity and a sign of protection. They provided a layer of protection against the spread of the virus, it became mandatory in most settings, and were mass-manufactured to address the urgent need. But new research indicates the same masks that protected us throughout the pandemic can now be leaving a toxic trail behind.
A paper by scientists at Coventry University, published in Environmental Pollution, has established that disposable masks are leaching microplastics and toxic chemicals, such as endocrine disruptors, into the environment. This chemical fallout could have long-term impacts on human health, wildlife, and ecosystems globally, scientists warn.
During the height of the pandemic, the world consumed a projected 129 billion single-use face masks monthly. The majority were composed of polypropylene and other plastics and were meant to be used once and then discarded. Without a proven recycling stream, they wound up in landfills, scattered on urban streets, or carried by rain into rivers and oceans.
Also Read: Could A Daily Pill Restore Brain Function After Stroke? Scientists Test Bold New Treatment
These masks have started to degrade over time. Field studies in recent times have reported abandoned masks in soil, on beaches, in water bodies, and even in rural areas far from civilization. As they disintegrate, they do not vanish—they scatter tiny fragments of plastic and chemical additives in the environment.
Dr. Anna Bogush, the lead author of Coventry University's study, refers to this as a pressing problem. "We can no longer overlook the environmental price of single-use masks, particularly when we have learned that the microplastics and chemicals they emit have a detrimental impact on human beings and ecosystems alike," she stated.
Why Testing the Disposed Masks Is Essential?
To find out what happens to masks when they disintegrate, Bogush and co-researcher Dr. Ivan Kourtchev did a simple but insightful experiment. They put fresh, unused masks—surgical masks as well as filtering facepieces like FFP2 and FFP3—into glass flasks of distilled water. The water was filtered after 24 hours at room temperature and then tested using sophisticated laboratory methods.
The findings were alarming. Each mask, whether it was a surgical, cloth or respirator, emitted microplastics. But filtering facepieces, commonly sold as the most effective level of protection amid the pandemic, lost four to six times more particles than basic surgical masks.
Most of them were small—less than 100 micrometers, about the diameter of a human hair—and consisted mainly of polypropylene. Small amounts of polyethylene, polyester, nylon, and PVC were present. These substances do not biodegrade readily, so they linger for decades in the environment.
Invisible Pollutants With Visible Consequences
The worry is not limited to plastics. The study found that masks also emitted chemical additives, such as Bisphenol B (BPB), a chemical that has been found to act like estrogen and interfere with hormonal systems in humans and animals.
The scientists estimated that at the peak of the pandemic, disposable masks released between 128 and 214 kilograms of BPB into the environment. That might seem insignificant compared to global levels of pollution, but the total effect of endocrine-disrupting chemicals—no matter how low the dose—has been found to influence fertility, development, and hormone function in humans and wildlife.
Microplastics, similarly, are not inert trash. When ingested by fish, birds, or small animals, they can become concentrated further up the food web, finally ending up in human diets. Microplastics have already been detected in seafood, tap water, and even in human lungs and blood.
Why Are These Disposable Masks Now Posing A Risk To Human Health?
The threats from microplastics and endocrine disruptors are multifaceted and as yet not fully appreciable, but the preliminary evidence is alarming.
Hormonal interference: Substances such as BPB have the potential to disrupt reproductive health, fetal growth, and metabolism.
Breathing difficulties: Microplastics inhaled through air can settle in lung tissue, leading to inflammation or other respiratory disorders.
Contamination of the food chain: Plastics carried by rivers, oceans, and land can contaminate crops and animals, with the risk of exposing individuals through food intake.
Scientists emphasize that this is not a standalone problem. Disposable masks are one part of a broader plastic pollution plague, which already encompasses bottles, bags, packaging, and man-made fabrics. But the unprecedented rate at which masks were used during the pandemic generated a shock and intense period of pollution.
Disposable Face Masks Have An Environmental Burden That Lingers
In contrast to biodegradable trash, the plastics found in disposable masks resist natural decay. One mask might take decades to degrade, releasing microplastics and chemicals along the way. For already plastic-stressed ecosystems, masks provide another source of stress.
Wildlife scientists have documented instances of animals getting tangled up in mask straps or eating shredded pieces. Marine ecosystems are especially at risk, since microplastics can settle into sediment and wreak havoc on entire food webs.
The environmental effect isn't quite even, however. Low- and middle-income nations, which frequently do not have effective waste management systems, bear a disproportionate weight of mask pollution.
The authors of the study contend that society must reexamine mask production, usage, and disposal. Single-use masks may have been necessary amid a peak health emergency on a global scale, but to continue using them without sustainable options threatens long-term damage.
The pandemic compelled billions of individuals to shift toward protective behaviors in one night. Masks helped save lives, safeguarded frontline health staff, and contributed significantly in slowing down the transmission of COVID-19. But their environmental legacy serves as a reminder that timely solutions to one crisis can generate new problems unless sustainability is made a part of the equation.
As the world prepares to face the next public health threat, safety gear can't be designed to be as if it stops with the disposal. The decisions we make today regarding manufacturing, using, and throwing away will resonate for decades in the environment and in our bodies.
Disposable masks were probably necessary in 2020, but by 2025, they are also a harsh reminder that each protective act has an unseen price tag. The only question is whether we will take action on this information before the chemical timebomb ticks again.
International Fetal Alcohol Syndrome Day 2025: Themes, Significance And History
Credits: Canva
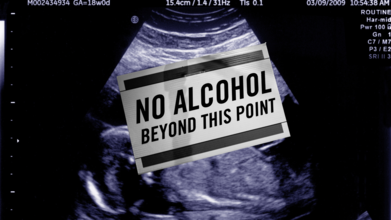
September is globally recognized as Fetal Alcohol Spectrum Disorder (FASD) Awareness Month, with September 9 dedicated to International FASD Awareness Day. This year, 2025, carries the powerful theme “Everyone Plays a Part: Take Action!”, a reminder that preventing FASD and supporting those affected is a collective responsibility.
What is FASD and Why It Matters
Fetal Alcohol Spectrum Disorder (FASD) describes the lifelong effects on the brain and body of a baby exposed to alcohol during pregnancy. It can lead to physical, behavioral, and cognitive challenges that persist throughout life. The most severe form, fetal alcohol syndrome (FAS), is characterized by distinct facial features, slow growth, learning difficulties, and developmental delays.
Also Read: Kissing Bugs Disease Could Soon Become An Endemic, Says CDC
FASD Theme 2025
This year’s theme, “Everyone Plays a Part: Take Action!”, is a call to collective responsibility. It highlights that FASD prevention is not just about individual choices but also about community support, healthcare education, and creating safe environments for expectant mothers.
Health professionals are encouraged to screen for alcohol use early in pregnancy, families are urged to provide support to those struggling with alcohol dependence, and policymakers are called upon to ensure inclusive systems for people with FASD. The message is simple yet powerful: prevention and support require all of us.
Experts emphasize that there is no known safe amount of alcohol to consume during pregnancy. Alcohol passes through the placenta to the developing baby, where it can cause permanent brain damage and affect organ development.
Also Read: What Role Do Genes Play In Alcoholism?
Symptoms vary, some children may face intellectual disabilities, behavioral issues, or difficulty with learning and social interaction. Others may experience challenges with coordination, speech, and growth.
The disorder is entirely preventable by avoiding alcohol during pregnancy. However, for those already living with FASD, early diagnosis and intervention can help manage symptoms and improve quality of life.
How FASD Awareness Day Began
International FASD Awareness Day was first observed on September 9, 1999, thanks to the efforts of parents and advocates like Bonnie Buxton, Brian Philcox, and Teresa Kellerman. They chose 9/9/99 to symbolize the nine months of pregnancy, a clear reminder that avoiding alcohol throughout those months can prevent FASD entirely.
What started as a grassroots effort in Canada and the United States has grown into a global movement. Communities worldwide now hold events, educational workshops, and social media campaigns each September to raise awareness, combat stigma, and advocate for better support systems.
Why This Day Matters
FASD Awareness Day is more than an observance, it is a global reminder that thousands of children are still born each year with preventable conditions linked to alcohol exposure. Beyond prevention, the day pushes for better understanding and empathy toward individuals already living with FASD. Stigma often keeps families from seeking help, and awareness campaigns aim to break that silence.
As the world observes FASD Day 2025, the message is clear: by spreading awareness, encouraging alcohol-free pregnancies, and supporting those affected, society can take a step closer to ending preventable harm and building inclusive communities where individuals with FASD can thrive.
Kissing Bugs Disease Could Soon Become An Endemic, Says CDC

Credits: Texas A&M University
The Centers for Disease Control and Prevention (CDC) report could be declaring the kissing bug disease or the Chagas disease an endemic in the United States.
But, before we jump into the report, let us understand the difference between an outbreak, endemic, epidemic, and pandemic.
Outbreak: As per the National Collaborating Centers for Infectious Disease, Canada, an outbreak is limited to a specific area, for instance a school, a department store, etc. and it is within a certain time period.
Endemic: The CDC notes that the amount of a particular disease that is usually present in a community is called an endemic. It is also called a baseline. The National Collaborating Centers for Infectious Disease says that an endemic is when it is always present in a geographical area or a population group.
Epidemic: The CDC notes that an outbreak becomes are epidemic when there is a sudden increase in the number of cases of a disease above what is normally expected in that population in a specific area. It can also spread to a larger area, for instance, within the country.
Pandemic: The CDC notes that when an epidemic spreads over several countries and continents, affecting many people, it is called a pandemic.
What Does The CDC Report Say?
In a report published last month in the September issue of the CDC’s Emerging Infectious Diseases journal, researchers highlighted that the disease is already considered endemic in 21 countries across the Americas. They also emphasized that growing evidence of the parasite’s presence in the United States is beginning to challenge the long-standing classification of the country as “non-endemic.”
The report stated that autochthonous, meaning locally acquired, human cases have been confirmed in eight U.S. states, with Texas reporting the highest number of cases. “Labeling the United States as non-Chagas disease-endemic perpetuates low awareness and underreporting,” the authors warned, further pointing out that the insect responsible for transmitting the disease has been detected in 32 states.
In addition to Texas, the other states where human cases have been identified include California, Arizona, Tennessee, Louisiana, Missouri, Mississippi, and Arkansas.
The report points out that available data is still “inadequate” to conclusively demonstrate whether the insects are expanding in either their geographic range or overall numbers. However, it also highlights that these bugs are being “increasingly recognized,” largely because of their frequent encounters with humans and the growing focus of scientific research.
“Invasion into homes, human bites, subsequent allergic reactions or exposure to T. cruzi parasites, and the rising number of canine diagnoses have all contributed to greater public awareness,” the report stated.
Read: What You Need To Know About Chagas Disease, Is it Contagious?
What Is The Kissing Bug Disease or The Chagas Disease?
Globally, around 8 million people are estimated to be living with Chagas disease, and about 280,000 cases are believed to exist in the United States, many of them undiagnosed.
Transmission occurs when the bug bites and then leaves parasite-containing droppings near the bite site. If a person accidentally rubs or scratches the area, or if the droppings come into contact with the eyes, mouth, or a cut in the skin, the parasite can enter the body and cause infection.
© 2024 Bennett, Coleman & Company Limited

